Table of contentIn this article
- When should I see a doctor for allergies?
- When to see your primary care doctor
- When you should see an allergist
- When you can use telehealth
- Signs that you should see a doctor
- How doctors can help with your allergies
- What can an allergist do for our allergies?
- Questions doctors will ask you about your allergies
- How you can help relieve allergy symptoms
- How Doctor on Demand can help with your allergies right now
- Doctor-answered allergy FAQs
You can manage many allergy symptoms on your own, but sometimes seeing a doctor or an allergist makes a real difference. Learn when to get medical help and when home care is enough. Explore how telehealth can help you get relief quickly.
When should I see a doctor for allergies?
You should see a doctor for allergies if your symptoms last more than a few weeks, interfere with your sleep, work, or daily routine, or aren’t getting better with over-the-counter treatment. A doctor can also help figure out if your symptoms are caused by allergies or something else, like a cold, and recommend the right treatment.
Allergies can cause a wide range of unpleasant symptoms, but it’s not always clear when you should manage them yourself or see a doctor.
Here are some signs that it might be time to talk to your doctor about your allergies:
- Your allergies are affecting your quality of life.
When allergies start disrupting your life, it’s time to see a doctor. If your symptoms affect your sleep, routine, exercise, or work, a doctor can help you manage them and get you back to feeling like yourself.
- Unclear symptoms that might not be allergies.
If you’re not sure whether allergies are causing your symptoms, a doctor can help test and diagnose the issue. For example, a doctor can help differentiate allergy symptoms from a common cold.
- Symptoms last for several months without improving.
If your allergy symptoms linger for weeks or months without improving, it’s worth seeing a doctor. Even if you can’t avoid the trigger, treatment can help you feel more comfortable and in control of your health.
- You are experiencing serious complications.
If your allergy symptoms are accompanied by more serious issues, like swelling, chronic sinus infections, or difficulty breathing, you should immediately see a doctor for medical care.
- Your symptoms aren’t going away with over-the-counter (OTC) medication.
If OTC medications like Claritin or Benadryl aren’t helping, or you can’t handle common side effects like drowsiness, it’s time to talk to a doctor. They can recommend other treatments that may be more effective or easier to tolerate.
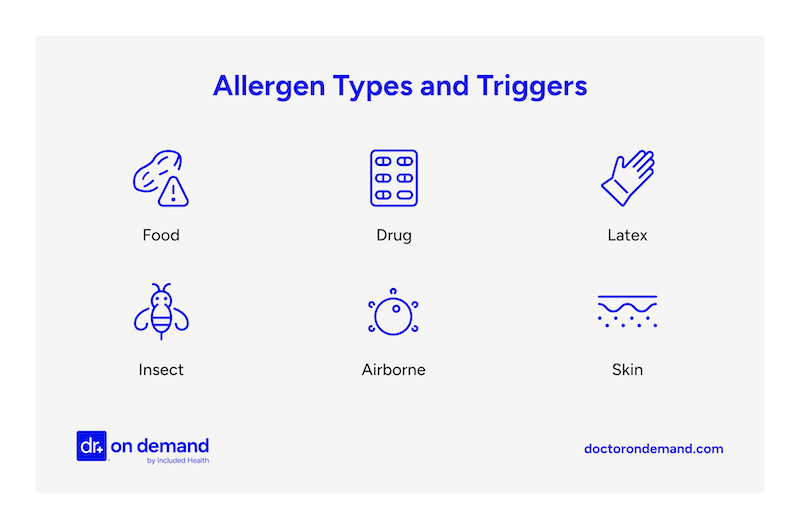
- You suspect a food, drug, or insect allergy.
Food, medication, and insect allergies can cause serious reactions. If you think one of these might be the cause, see a doctor soon for an allergy test. A doctor can also help you create an emergency plan that could be life-saving in case of a serious allergic reaction.
- You have other health issues, and you’re not sure how OTC medications will affect them.
If you have other health issues like asthma, atopic dermatitis (eczema), heart problems, or high blood pressure, you should check with a doctor before using certain allergy medications. They can help you choose safe options.
When to see your primary care doctor
Your primary care doctor is your first point of contact for diagnosing and managing mild allergy symptoms. They can assess your condition, prescribe a treatment plan, and refer you to an allergist if they feel you need specialized care.
Here’s when you should consider seeing your primary care doctor:
- Managing first-time symptoms of seasonal or mild allergies
Allergies can begin at any age. You may not know if your symptoms are due to allergies, a cold, or something else, but a doctor can help you figure it out and recommend the right treatment.
- Managing new symptoms of known allergies
Even if you’ve managed your allergies for years, symptoms can sometimes get worse. If your typical seasonal allergies feel harder to control, it’s worth seeing your primary care doctor to update your treatment plan. Your doctor can also assess if your symptoms point to a new trigger.
- Looking for a referral to an allergist
If your symptoms are severe, complex, or not responding to basic treatment, your doctor can refer you to an allergist for specialized testing and care. Many insurance plans require a referral for coverage.
- Discussing options for over-the-counter (OTC) or prescription treatments
Your primary care doctor knows your health history best and can guide you on which OTC medications or lifestyle changes might work best for you. They can also prescribe stronger treatments if necessary.
When you should see an allergist
See an allergist if your symptoms don’t get better with regular treatment, if you’ve had a serious reaction like anaphylaxis, or if you want long-term relief from allergy shots or tablets. Allergists can also find out what you’re allergic to and help treat related issues like asthma or eczema.
Here’s a closer look at when you should consider seeing an allergist:
- Primary care isn’t helping, and symptoms are persistent.
If your symptoms aren’t responding to typical treatments, are ongoing, or are severe, an allergist can help you find a more effective solution.
- You have asthma or eczema.
Allergies can make conditions like asthma or eczema worse. An allergist can help manage all of these with a treatment plan that controls symptoms.
For people with severe asthma triggered by allergies, a doctor may also discuss “asthma biologics.” These are advanced medications that block specific immune signals that lead to inflammation. The goal is to reduce asthma attacks in people who don’t respond well to conventional treatments.
- You want an allergy test.
Allergists can perform allergy testing, like skin pricks or blood tests, to determine what’s causing your symptoms. They can check for pollen, mold, dust mites, pet dander, and cockroaches (their saliva, droppings, or dropped body parts). They can also test for insect stings or venom allergies.
If you need testing for food allergies, it’s really important to see an allergist. They can safely supervise oral food challenges if there is uncertainty about a suspected food allergy and no safer testing alternatives exist.
- You’re interested in immunotherapy treatment (allergy shots or sublingual tablets).
An allergist can offer immunotherapy if you have allergies that don’t improve with medication. This approach helps your body build tolerance to allergens over time. Usually, patients must receive regular treatment over three to five years to build long-term tolerance.
There are two main types of immunotherapy:
1. Allergy shots: An allergist gives you small doses of the allergen that triggers your symptoms, like pollen, dust mites, or pet dander. Eventually, your sensitivity lessens and your symptoms improve. Over a few years, the allergist slowly increases the dose to build tolerance.
2. Sublingual tablets: For some airborne allergens (like ragweed, certain grasses, and dust mites), doctors may offer tablets that go under your tongue. The patient can take these at home, but the allergist monitors the dose and timing. Like allergy shots, they’ll slowly increase the dose to help your body build tolerance.
Immunotherapy is especially helpful for people with long-term allergic rhinitis (hay fever), which causes symptoms like nasal congestion, sinus pressure, sneezing, headaches, and trouble breathing. For people with moderate to severe allergic rhinitis, these symptoms can seriously affect daily life, but immunotherapy can offer lasting relief.
A 2022 study in The Lancet Regional Health – Europe looked at the long-term impacts of allergy shots on thousands of people with allergic rhinitis. The paper, titled “Long-term real-world effectiveness of allergy immunotherapy in patients with allergic rhinitis and asthma: Results from the REACT study, a retrospective cohort study,” showed that allergy shots helped reduce symptoms for up to nine years after starting treatment. People also needed fewer allergy medications over time and reported better sleep, improved focus at work or school, and experienced an overall boost in well-being. The study also found that although immunotherapy patients had higher upfront costs, they made up for it over time. As their symptoms improved, they needed fewer hospital visits and used less medication, leading to long-term savings.
- You’ve had severe allergic reactions (e.g., anaphylaxis, swelling).
After a serious allergic event, such as anaphylaxis, seeing an allergist is essential to understand your risks and develop an emergency plan.
- You suspect you have a food, medication, or insect allergy.
If you notice an allergic reaction after eating certain foods, taking medications, or getting stung by an insect, see an allergist. They can test for specific allergies, identify your triggers, and help you create a clear plan to avoid serious reactions in the future.
It’s particularly important to see an allergist if you suspect food, drug, or insect allergies. These allergies can sometimes cause severe or even life-threatening reactions if you don’t properly manage or identify them.
When you can use telehealth
Use telehealth for routine follow-ups and managing medications or prescriptions. You can also schedule an initial consultation to discuss your symptoms and concerns. Afterward, you and your doctor can decide whether you need an in-person evaluation.
Telehealth offers patients a convenient way to support follow-up care and medication management for many mild allergies. During these appointments, the patient and doctor connect over a video call. The doctor uses a high-quality internet connection to see important areas like your throat, skin, or eyes. They also ask questions about your medical history and symptoms.
A 2016 study, “Synchronous Telehealth for Outpatient Allergy Consultations” from the Annals of Allergy, Asthma & Immunology, found that doctors were able to manage conditions like allergic rhinitis, asthma, urticaria, and drug allergies through video visits. In that study, only 2 of the 37 patients needed an in-person follow-up. The authors concluded that telemedicine is a viable treatment for many routine allergy cases.
A 2022 study, “The Future of Telehealth for Allergic Disease” from The Journal of Allergy and Clinical Immunology: In Practice, also found that many patients had positive experiences using telehealth to manage their allergies.
Here’s when to consider telehealth for allergies:
- You have mild to moderate allergy symptoms.
If you’re experiencing typical allergy symptoms like sneezing, runny nose, or itchy eyes, a telehealth visit can help you get advice and treatment. If you have more complex symptoms, like a spreading rash, hives, or trouble breathing, it’s better to get an in-person consultation.
- Refills for allergy medications
Telehealth doctors can prescribe or renew any medications you need, without you having to travel to an in-person office.
- Initial consultation or screening
A doctor can review your medical history, talk through your symptoms and when they get worse or better, and perform a virtual exam to help identify and manage allergies. They can suggest ways to reduce exposure and prescribe medication if needed.
- Follow-up visits
After your first in-person visit, you can often schedule virtual follow-ups so your doctor can check your progress and adjust your treatment if needed.
- You live in a remote area.
If you don’t have easy access to a specialist, you can often start with a telehealth appointment from home. After the first visit, you and the doctor can decide if traveling for in-person care is necessary.
When to go to urgent care
Go to urgent care if you need fast treatment for allergy symptoms that are severe but not life-threatening, like a sudden rash, mild swelling, hives, or difficulty breathing. Urgent care clinics can provide rapid treatment and monitoring so the issues don’t escalate.
Urgent care centers are open 24/7/365. They’re a good option if you want fast relief for concerns, moderate to severe allergic reactions, without waiting for a regular doctor’s appointment.
Here’s when to go to urgent care for allergic reactions:
- Moderate swelling in your face, throat, or mouth
Food, insect, or medication allergies can cause your face, throat, and lips to swell. Mild swelling can worsen, so a doctor should check it early to prevent serious breathing problems.
- Difficulty breathing
If your throat and chest hurt to the point that you’re short of breath, but you’re not gasping or wheezing, urgent care doctors can help you quickly manage your symptoms, monitor your condition, and prevent the situation from worsening.
- Severe diarrhea from food allergies
Food allergies can cause intense stomach reactions that can lead to dehydration if you don’t get quick treatment.
- Sinus infection
Allergies can block your sinuses and cause sinusitis (sinus infections), which may require antibiotics or other treatments.
- Severe hives or a rash that spreads quickly
A fast-spreading rash can indicate that your allergic reaction is escalating and may need urgent medical attention.
- Rapid heart rate
Allergies can sometimes trigger a fast heartbeat. Urgent care can check your heart rate and make sure you stay stable.
When to call 911
Call 911 immediately if you suspect anaphylaxis, a rapid-onset allergic reaction that can cause full-body shock and lead to death. If you experience life-threatening symptoms, like severe trouble breathing, major swelling, or a rapid heart rate, call 911. Fast treatment can save a life, even if symptoms initially seem mild.
Even if you use an epinephrine injector and feel better afterward, you should still call 911. Symptoms can return suddenly, and emergency care is still needed.
If you experience any of the following after exposure to an allergen, call 911 instead of trying to drive yourself to the hospital:
- Suspected anaphylaxis (even if symptoms appear mild)
Anaphylaxis is a severe allergic reaction, often triggered by food, medications, insect stings, or latex. It can get worse very quickly and cause life-threatening symptoms like a fast heartbeat, severe swelling, and trouble breathing. If you suspect anaphylaxis, call 911 immediately.
- Trouble breathing or shortness of breath
If you have difficulty breathing suddenly, your throat or airways may be closing. This reaction can quickly escalate to a medical emergency requiring immediate care to ensure you can continue breathing.
- Swelling of the face, lips, tongue, or throat
If your tongue, throat, or face swells, it can block your airway and restrict your breathing.
- Sudden drop in blood pressure (feeling dizzy or confused)
It could be a sign of shock if you suddenly feel faint, dizzy, or confused. This means your body isn’t getting enough blood to vital organs and needs emergency treatment.
- Rapid pulse or dizziness
If your pulse suddenly starts racing, it may be a sign that your body is in shock. Without quick treatment, you could faint or collapse.
- Severe skin reactions like hives all over the body
Widespread, fast-spreading hives can indicate that the reaction is affecting your whole system, not just your skin. This situation can quickly escalate to a medical emergency.
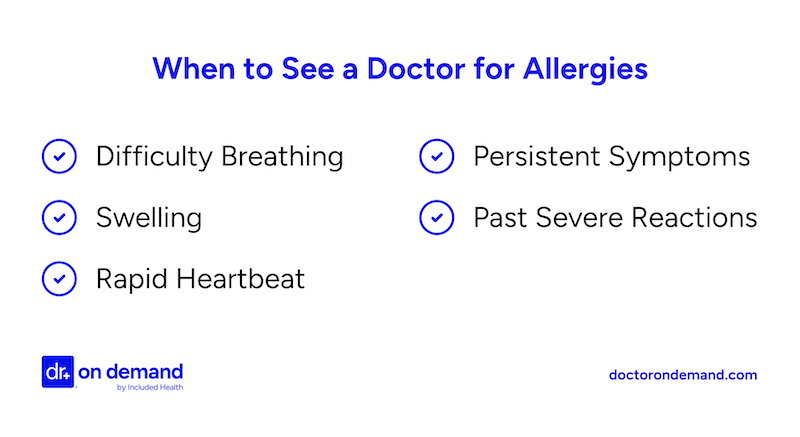
Signs that you should see a doctor
See a doctor if your allergies make it hard to get through the day or sleep well. Also, serious symptoms like trouble breathing, swelling, rashes, or sinus problems all need medical attention. Even mild symptoms that don’t go away might need a doctor’s help.
Here’s a list of symptoms that indicate it’s time to see a doctor for your allergies:
- Shortness of breath and related symptoms
See a doctor if you’re having trouble breathing, wheezing, coughing a lot, or feeling tightness in your chest. These could be signs that you’re developing asthma or having a more serious allergic reaction.
- Frequent sinus or ear problems
Recurring sinus or ear infections can be related to unmanaged allergies. A doctor can help treat the acute issue and help prevent future flare-ups.
- Severe reactions (hives, swelling, gastrointestinal issues)
Get medical attention right away if you have hives, facial swelling, stomach pain, or trouble breathing. These are signs of a serious allergic reaction that could escalate to life-threatening conditions without treatment.
- Eye symptoms that are persistent or very uncomfortable
Red, itchy, watery eyes are common symptoms of seasonal allergies. However, if your symptoms are long-lasting, cause significant discomfort, or are affecting your vision, see a doctor. They can rule out eye infections or other potential causes.
- Symptoms that disrupt our sleep
If congestion, coughing, or postnasal drip keeps you up at night, a doctor can help you find the right treatment to sleep well.
- Symptoms that aren’t resolving with time or OTC medications
Even if your symptoms seem mild, it’s worth seeing a doctor if they last more than a few weeks or don’t improve with over-the-counter medicines. A doctor can prescribe different medications or help you make lifestyle changes that dramatically relieve discomfort and improve your quality of life.
- Allergy symptoms that trigger other conditions
Allergies can trigger other conditions like asthma and eczema. Doctors can help manage both conditions together and reduce flare-ups.
- Worsening symptoms in children
If your child starts having new or ongoing symptoms, like snoring, mouth breathing, or frequent ear infections, it could be a sign of allergic rhinitis. Treating it early may help prevent asthma from developing later.
How doctors can help with your allergies
Doctors can test for allergy triggers and recommend medications or lifestyle changes to manage your symptoms. They can also refer you to allergists and create a long-term plan to help you keep your allergies under control.
How doctors can help with your allergies:
- Confirm whether symptoms are due to allergies or another condition.
- Recommend appropriate treatments (OTC or prescription).
- Prescribe emergency medications if needed (e.g., epinephrine auto-injectors).
- Offer allergy testing to identify specific triggers.
- Provide guidance on environmental controls and prevention.
- Develop long-term management plans.
Dr. Ashley Kelley from Included Health shares, “I often have patients come to see me who have tried various over-the-counter antihistamines and nasal sprays but are still struggling with daily allergy symptoms such as itchy eyes and nasal congestion. It’s helpful at this point to take a step back and try to identify what may be causing the symptoms and try to limit exposures when possible. Depending on the patient’s individual situation, we may try avoidance plans such as limiting time outdoors on high pollen count days, or removing throw pillows, curtains and rugs from bedrooms. I often will also refer my patients to allergy testing so we can better understand which allergens to focus on.”
What can an allergist do for our allergies?
Allergists help you control your allergies so they don’t affect your daily life. They can find out what you’re allergic to, create a treatment plan that fits your needs, give allergy shots for severe cases, and help manage related problems like asthma.
Board-certified allergists are doctors with specialized training in diagnosing and treating allergies and other immunological conditions. While mild allergies often don’t require a specialist, allergists are the best choice for identifying triggers, managing severe allergies, or treating cases where symptoms don’t improve with standard care. They can provide more comprehensive testing and treatment options than primary care doctors.
Here’s an overview of how allergists can help with your allergies:
- Allergy testing
Allergists can determine whether your symptoms are caused by a specific allergy or something else. They may use skin prick tests, blood tests, or oral food challenges depending on what they suspect. These diagnostic tools help precisely identify the allergen triggering your symptoms, which helps them develop more accurate treatment plans.
- Provide personalized treatment plans
Once your allergist identifies the cause of your allergies, they can work closely with you to develop a personalized plan. For example, they can prescribe and adjust medications to control symptoms effectively. They might also suggest lifestyle changes, such as staying indoors during peak pollen times or adjusting your home environment to reduce triggers like dust mites, pet dander, or mold.
- Offer immunotherapy (allergy shots or sublingual tablets)
If avoidance and medications aren’t enough, allergists can perform immunotherapy, such as allergy shots or sublingual tablets. Immunotherapy can help retrain your immune system to become less reactive to allergens. Though the process takes several years, it usually offers long-term relief.
- Help patients manage overlapping conditions
Many people with allergies also have problems like asthma, eczema, or sinus issues. Allergists can help manage all these conditions together, not just the allergies. They can also work to coordinate care with other doctors if your case is more complex.
- Educate patients on reducing exposure
An allergist can also help you understand how to limit exposure to allergens at home, work, and outdoors. Avoiding allergens is one of the most effective ways to prevent an allergic reaction.
- Help you prepare for emergencies
Allergists can teach you how to recognize severe signs of anaphylaxis and teach you how to administer emergency medications, like epinephrine shots, to yourself and others.
Questions doctors will ask you about your allergies
Doctors will ask questions to figure out what’s causing your allergies and how to treat them. They might ask when your symptoms started, what triggers make them worse, and whether you have other health conditions that could affect your treatment.
When you visit a doctor about allergies, it helps to come prepared with notes about your symptoms, possible triggers, and any relevant medical history.
Here are some questions your doctor might ask:
Symptoms:
- What symptoms are you experiencing? Are they mild or moderate?
- When did your symptoms start?
- Do they happen year-round, or only during certain seasons?
- What time of day are they usually worse?
Your triggers:
- What seems to make your symptoms worse (pollen, pets, dust, food, exercise, etc.)?
- Do your symptoms happen indoors, outdoors, or both?
- Have you recently traveled, moved, or changed environments?
- Do you have pets at home, or are you exposed to other common allergens?
Your health history:
- Have you had allergies before? If so, have they changed?
- Do you have a history of asthma, eczema, or sinus issues?
How you can help relieve allergy symptoms
The best way to relieve allergy symptoms is to limit your exposure to the trigger, whether it’s pets, food, pollen, or something else. You can also manage symptoms with antihistamines, prescription medications, and changes to your home and daily routine.
Here’s how you can help prevent common allergy symptoms and manage them when they do happen:
- Keep windows closed.
- Change clothes when coming in from outside.
- Shower and wash your hair before going to bed.
- Don’t air-dry clothes outside.
- Use an air filter with a HEPA filter.
- Keep windows closed during high pollen seasons.
- Use HEPA filters in your home.
- Shower and change clothes after spending time outside.
- Avoid known triggers (e.g., pets, certain foods).
- Use antihistamines or decongestants as recommended.
- Rinse sinuses with saline spray or a neti pot.
- Wash bedding and vacuum frequently.
- Dr. Kelley recommends, “More frequent vacuuming for certain patients with allergies is necessary. Patients who have moderate to severe allergies, especially to dust or pet dander, may consider washing sheets every week and vacuuming 2-3 times per week.”
- Monitor pollen counts and stay indoors when levels are high.
How Doctor on Demand can help with your allergies right now
A Doctor On Demand virtual visit connects you with a licensed provider anytime you need help with your allergies. Whether you’re dealing with sneezing, congestion, itchy eyes, or something else, you can receive help in minutes. Get expert advice, a diagnosis, and prescriptions without ever leaving home.
Whether it’s your first time dealing with allergies or you’ve been managing them for years, Doctor on Demand can help. You can log into our 24-hour virtual urgent care for immediate support or book a same-day appointment, all without the waiting room or travel.
A licensed Doctor on Demand provider will review your allergy symptoms and ask about possible triggers like pollen, pets, dust, or certain foods. They’ll provide a diagnosis, adjust or refill medications if needed, and guide you on the best next steps. If your symptoms suggest you need specialist care, they can refer you to a local allergist.
You can also revisit Doctor on Demand for convenient follow-ups or ongoing allergy management.
How to prepare for your Doctor on Demand telehealth visit for allergies
To get the most out of your virtual Doctor On Demand allergy visit, prepare to use your computer, tablet, or phone in a quiet, well-lit space. Be ready to talk about your symptoms and share when they started, what might be triggering them, and what treatments you’ve tried.
Here’s how to get ready for your Doctor on Demand virtual visit:
- Find a quiet, well-lit area for your appointment.
Choose a private location with good lighting so your doctor can see and hear you. Your doctor must be able to see and assess visible allergy symptoms, like red eyes and rashes.
- Confirm your tech works.
Make sure your internet connection is strong and your camera and microphone are working. It’s a good idea to test the Doctor On Demand platform in advance and keep your device charged or plugged in during the visit. You don’t want your call to drop because your device’s battery is running low.
- Be ready to discuss symptom details.
Before the appointment, think back on your allergy symptoms. Write down when they started, how often they happen, and what makes them better or worse. Include any other relevant details specific to your situation. For example, what has changed if you’ve managed allergies on your own for years but now can’t? Also, write down medications and dosages you’re taking. This helps your doctor understand your situation and recommend the best next steps.
- Take notes.
Take notes during your visit to remember any key treatment advice and follow-up instructions.
Doctor-answered allergy FAQs
Get answers from doctors about allergy symptoms and treatment. Find out when you should see a doctor and when you can manage symptoms on your own. You’ll also learn how to tell the difference between allergies and a cold, and more.
- When should I be concerned about my allergies?
You should be concerned about your allergies if they affect your daily life, especially your sleep. Also, watch out for serious symptoms like shortness of breath, swelling, rashes, or hives. These all require medical attention to treat and manage.
- How can a doctor tell if you have allergies?
A doctor can diagnose allergies by performing an allergy test, doing a physical exam, and reviewing your symptoms and medical history. They may also ask if you think you have an allergy and if anything seems to make your symptoms worse.
- Can a doctor prescribe something stronger for allergies?
Yes, doctors can prescribe stronger allergy medications than typical over-the-counter drugs you can buy in the store. Allergists can also give allergy shots over time to help your body get used to an allergen.
- What kind of doctor does allergy testing?
Allergists and many primary care doctors can test for allergies to things like pollen or dust. For more serious allergies, like reactions to food or medicine, it’s safer to see an allergist because testing could cause a strong reaction.
- Can a doctor do anything for severe allergies?
Yes, doctors can help treat severe allergies. They can prescribe strong steroids or antihistamines to reduce symptoms like swelling, breathing problems, and hives. For very severe cases, they can administer allergy shots or sublingual therapy. Also, they will prescribe epinephrine (EpiPens) if there’s a risk of anaphylaxis.
- Is a doctor’s visit necessary when your ears are clogged from allergies?
Mild ear clogging usually doesn’t require a doctor’s visit. Over-the-counter antihistamines or decongestants can relieve the symptoms. See a doctor if the issue lasts more than a few days, is very painful, affects your hearing, or comes with a fever or other signs of infection.
- Will I need allergy shots?
You don’t need allergy shots if you have mild, seasonal allergies. But allergy shots might be a good option if you have moderate to severe environmental allergies that don’t get better with medication.
- Will I need a follow-up doctor’s appointment for allergies?
You’ll need a follow-up appointment if your symptoms don’t improve, get worse, or if you have side effects from your treatment. If your allergies are under control, a follow-up usually isn’t necessary.
- How can I tell the difference between allergies and a cold?
Allergies and colds can cause similar symptoms, like a stuffy nose and sore throat. Colds usually clear up in a week or two, while allergy symptoms can last longer or come and go. An allergy test can help confirm if allergies are the cause.
About the authors

Dr. Jeanette Carpenter is board certified in Family Medicine and practices in Virginia. She has an interest in preventative medicine and holistic medicine and has a certification in plant based nutrition from eCornell. She believes stress and lifestyle impacts the disease process and spends extra time educating patients on lifestyle modifications that can improve their overall health.

Quan Lam is a copywriter with over 15 years of experience writing and editing content for both start-ups and legacy brands, as well as 2 years of writing experience exclusively within the healthcare space. She currently lives and works in New York City.



