Table of contentIn this article
- When to go to urgent care for COVID-19
- When to go to the ER for COVID-19
- Recognizing COVID-19 symptoms before going to urgent care
- Common situations when urgent care is appropriate for COVID-19
- What to expect from a COVID-19 test at an urgent care
- Home treatments for mild COVID symptom management
- How Doctor On Demand can assist with COVID-19
- Doctor-answered COVID-19 FAQs
COVID-19 can feel overwhelming, and it’s not always clear when to see a doctor. Urgent care can help with testing, moderate symptoms, and treatment. Learn when a visit makes sense, what to do at home, and how telehealth can support your recovery.
When to go to urgent care for COVID-19
Go to urgent care if you have moderate COVID-19 symptoms and need testing or want to talk to a doctor. It’s also a good option for required tests for work or travel. If symptoms get worse or you’re high-risk, urgent care may offer treatments to help prevent complications.
In a 2022 paper, “Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19” from the Cochrane Database of Systematic Reviews, researchers explain that diagnosing the severity of COVID-19 based on symptoms alone can be difficult because the illness often mimics the common cold or flu. Like a cold or the flu, COVID-19 usually causes a combination of symptoms — not just a sore throat, fever, or cough, but several symptoms at once. The review also notes that doctors look beyond symptoms, considering whether a person has been exposed to someone with COVID-19 or has recently traveled to high-risk areas.
If you’re experiencing more than one symptom or have had a known exposure, it’s a good idea to visit urgent care. A provider can assess your symptoms, order a test, and help you decide on the next steps.
Here are more specifics about when to go to urgent care for COVID-19:
- You’re experiencing moderate COVID-19 symptoms and need quick support
If you’re experiencing symptoms like fever, cough, or fatigue and want to get tested or speak with a provider, urgent care can help, especially if you can’t reach your regular doctor. They offer same-day care and may prescribe treatment, particularly for high-risk patients.
- You have symptoms and want to get tested
Most urgent care clinics often offer both PCR and rapid antigen tests. PCR (Polymerase Chain Reaction) tests are more accurate, but results take longer. If you have symptoms and want to confirm whether it’s COVID-19, clinics can test you and guide you in your next steps.
- You need a COVID-19 test to travel
As of 2025, most places have lifted their COVID-19 testing requirements for entering buildings, traveling abroad, and more. However, there are still exceptions. In these cases, urgent care centers offer the most convenient place to get tested. They can perform a PCR test or a rapid antigen test, depending on how fast you need the results. While you’re there, the providers can also offer guidance on how to avoid getting sick while traveling.
- Evaluation for antiviral treatment eligibility
Urgent care clinics can evaluate whether you qualify for antiviral treatments such as Paxlovid. If you’ve tested positive and are at higher risk for severe illness — due to age, a health condition, or other factors — a provider may prescribe treatment. Urgent care is a practical choice if your regular doctor isn’t available quickly.
When to go to the ER for COVID-19
Go to the emergency room if you have severe symptoms like trouble breathing, chest pain, or a very high fever. These may be signs of serious complications, such as respiratory failure, that need immediate medical care. Don’t wait if symptoms are escalating quickly.
Some COVID-19 symptoms can cause life-threatening complications that require immediate medical treatment. In these cases, prompt treatment in an ER can be life-saving. If you or someone near you experiences any of the signs below, go directly to the nearest emergency room or call 911:
- Shortness of breath at rest, or severe or worsening difficulty breathing
Go to an ER or call 911 if you experience shortness of breath, especially if it occurs at rest, worsens, or makes speaking difficult. These signs may indicate low oxygen levels that can cause respiratory failure.
- Persistent chest pain or pressure
Chest pain or tightness is a sign of lung inflammation or a cardiovascular event.
- Sudden confusion, disorientation, or trouble staying awake
Call 911 if you or someone you know isn’t make sense while speaking, can’t recognize familiar people, or is falling asleep mid-conversation. These symptoms may signal dangerously low oxygen levels or a serious infection affecting the brain.
- Blue or pale lips or face
If your face or lips are somewhat blue, you may have dangerously low oxygen levels in the blood. If you suddenly develop this symptom in combination with other symptoms, like a shortness of breath, go to the ER.
- Moderate or worsening symptoms for high-risk individuals
If you’re in a high-risk group — such as being over 65, immunocompromised, or living with a chronic illness — even moderate COVID-19 symptoms may require emergency care. A worsening cough, rising fever, increasing fatigue, or a drop in oxygen levels can escalate quickly. For high-risk patients, early ER evaluation can be life-saving.
When you can use telehealth for COVID-19
Telehealth is a good option if you have mild symptoms and want to speak with a doctor. A provider can assess your condition, prescribe antivirals, and help you decide if in-person care is necessary, all without the risk of spreading COVID-19 in a clinic.
Since the start of the pandemic, telehealth has become a widely used tool for managing COVID-19 from home. It allows providers to guide you through many aspects of care, especially during the early stages of illness.
Telehealth isn’t right for emergencies. If you have severe symptoms — such as trouble breathing, chest pain, or confusion — you should go to the emergency room or call 911. But for many people, telehealth offers fast, safe, and effective support while recovering from COVID-19 at home.
Here’s how telehealth services can support COVID-19 recovery:
- Symptom assessment
A provider can evaluate the severity and progression of symptoms, such as fever, cough, or shortness of breath, and determine next steps.
- Testing guidance
Advising on the need for COVID-19 testing and interpreting results.
- Treatment plans
Depending on your symptoms and risk level, you may be eligible for antiviral medications such as Paxlovid. A provider can prescribe treatment or refer you to in-person care if necessary.
- Monitoring
Telehealth allows for regular check-ins throughout your recovery. This is especially helpful for people at higher risk of complications, such as older adults or anyone with chronic conditions.
Recognizing COVID-19 symptoms before going to urgent care
COVID-19 symptoms can range from mild to severe and often overlap with cold or flu symptoms. Common signs include fever, cough, fatigue, and sometimes a loss of taste or smell. If you’re unsure whether it’s COVID-19, urgent care can help confirm with testing.
COVID-19 symptoms appear two to 14 days after exposure to the virus. It’s important to monitor and recognize the symptoms closely, especially if you have underlying health conditions.
Here’s a list of common symptoms of COVID-19 that you might experience:
- Fever or chills
Most medical sources define a fever as a body temperature above 100.4°F (38°C). With COVID-19, fever often comes with chills, night sweats, or feeling flushed. Some people experience low-grade fevers that come and go, while others may spike higher. A high or persistent fever can be a sign of a more serious infection and should be checked by a provider.
- Cough
A dry, persistent cough is one of the most common COVID-19 symptoms. It often develops early in the illness and may linger for several days or even weeks, even after other symptoms improve.
- Shortness of breath or difficulty breathing
COVID-19 usually affects the lungs and makes breathing more difficult, especially during physical activity. If you’re having trouble catching your breath while resting or speaking in full sentences, you may have more serious respiratory distress and should visit urgent care.
- Fatigue
Fatigue is one of the most common and lingering symptoms. Many people feel extreme tiredness that doesn’t improve with rest. It can show up early in the illness or after other symptoms begin. Even mild cases of COVID-19 can cause days of low energy or mental fog, which may continue for a week or more.
- Muscle or body aches
Body aches often go hand-in-hand with fever and fatigue. These body aches usually improve as the fever goes down.
- New loss of taste or smell
A sudden loss of smell or taste is a unique symptom of COVID-19 that can develop even if no other symptoms are present. While some people regain these senses within a week, others may lose them for longer. This symptom can help distinguish COVID-19 from a cold or flu.
- Sore throat
A sore throat alone might just be a cold or irritation, but if it occurs alongside fever, cough, or body aches, it’s more likely part of a COVID-19 infection.
- Congestion or a runny nose
Nasal and sinus congestion are very common and may resemble symptoms of seasonal allergies or a regular cold. If the congestion occurs with fever or fatigue, it’s more likely to be COVID-19.
- Nausea or vomiting
Stomach-related symptoms are less common with COVID-19, but they do happen, especially in children and younger adults. These may include nausea, vomiting, or diarrhea, and often show up before classic respiratory symptoms such as coughing or shortness of breath. If you start with GI symptoms and later develop a fever, fatigue, or cough, it could be COVID-19. In these cases, getting tested can help confirm the diagnosis and guide treatment.
Mild symptoms of coronavirus
Mild symptoms of coronavirus include a low-grade fever and mild respiratory signs such as a cough or sore throat. You may also be tired and have a headache and congestion. Most people can recover from these symptoms at home without having to see a doctor.
Most individuals with mild symptoms can recover at home with supportive care, such as rest, hydration, and over-the-counter medications to relieve symptoms.
Here’s a list of mild COVID-19 symptoms that don’t require a trip to the doctor for most otherwise healthy people:
- Low-grade fever
A temperature around 99–100.4°F that doesn’t last more than a few days.
- Mild cough
A dry cough that isn’t painful or disruptive to breathing.
- Sore throat
You may have mild irritation or scratchiness when swallowing, but shouldn’t have swelling or white patches in your throat.
- Nasal congestion
You may have minor nasal congestion or a runny nose that’s similar to what you might feel from a common cold or seasonal allergies.
- Fatigue
Most people will feel tired and have low energy, even if they sleep enough.
If you’re managing these symptoms at home, monitor for any changes. If you develop new symptoms like difficulty breathing, chest pain, confusion, or a high fever that won’t go down, seek medical care right away. Likewise, people who are older or who have chronic health conditions should consider checking in with a provider, even for mild symptoms.
Symptoms that are signs you should seek emergency care
Some COVID-19 symptoms are medical emergencies. If you or someone you know has serious trouble breathing or persistent pain in the chest, go to the emergency room or call 911 immediately. Any delay can lead to serious complications and even death.
The following symptoms are signs of a medical emergency. If you or someone near you is experiencing these symptoms, go to the ER or call 911:
- Trouble breathing
You feel short of breath, even while resting or speaking.
- Persistent pain or pressure in the chest
Your chest feels tight, heavy, or painful, and it doesn’t go away.
- Disorientation, inability to wake up or stay awake
You’re unusually drowsy or struggling to stay conscious.
- Pale, gray, or blue-colored skin, lips, or nail beds
Blue, pale, or gray skin may signal dangerously low oxygen.
If you or someone you are caring for exhibits any of these symptoms, seek emergency medical care immediately.
Common situations when urgent care is appropriate for COVID-19
Urgent care clinics are a good option for COVID-19 concerns that need timely attention but aren’t life-threatening. They’re also a convenient place to get rapid testing — whether you’re experiencing symptoms, were recently exposed, or need documentation for work, school, or travel.
Here are common COVID-19 scenarios where urgent care is a smart option:
- Mild symptoms are getting worse, not better
If your mild COVID-19 symptoms, such as cough, fatigue, or fever, worsen after a few days, it’s worth checking in with a provider. Urgent care can evaluate your symptoms, monitor your condition, and intervene quickly with treatment if needed.
- You’ve been exposed to COVID-19
If you’ve been in close contact with someone who tested positive, urgent care is a convenient place to get tested, even if you feel fine. Quick results can help you make informed decisions and avoid spreading COVID-19 to your family, friends, co-workers, and community.
- Need quick test results to return to work or school
Some employers or schools may still require proof of a negative COVID-19 test after illness or exposure. Urgent care centers can often provide same-day testing and documentation you need.
- Symptoms with a pending travel plan
If you’re feeling unwell but have upcoming travel plans, urgent care can help determine whether it’s safe to go. Providers can test for COVID-19 and advise whether you should delay or cancel your trip to avoid spreading infection.
- Assessment for antiviral treatment
Some urgent care clinics can assess whether you qualify for treatments like Paxlovid. These medications work best when started within five days of symptom onset. Urgent care clinics offer the timely evaluation needed to get the most out of the medication.
COVID-19 High-risk groups
People in high-risk groups are more likely to develop severe or life-threatening complications from COVID-19. This includes adults 65 and older, immunocompromised individuals, and pregnant people. High-risk individuals should monitor their symptoms closely and seek medical care early.
COVID-19 high-risk groups include:
- Older adults
According to the Centers for Disease Control (CDC), age is the strongest risk factor for severe COVID-19 complications. For example, the risk of hospitalization and death increases significantly after age 65.
In a 2022 paper, “Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality” from the Journal of Clinical Medicine, individuals 65 years and older accounted for more than 80% of hospitalizations. They had a 23 times higher risk of death compared with those aged 18 to 29 years.
- People with underlying medical conditions
Certain diseases and health conditions make people more likely to get very sick from COVID-19 because the conditions weaken them. They may need more aggressive monitoring if they’re infected. According to the CDC, the following diseases and conditions put you in a high-risk group for severe illness:- Cancer
- Cerebrovascular disease, like stroke
- Chronic kidney disease
- Chronic liver disease
- Chronic lung disease (including moderate to severe asthma)
- Cystic fibrosis
- Type 1 and 2 Diabetes
- Heart conditions
- Hemoglobin blood disorders (e.g., sickle cell disease)
- Obese people
According to the 2020 paper “Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality,” people who may be considered obese are up to twice as likely to end up in the hospital or ICU compared with those who aren’t.
- Smokers
In the same 2020 paper, the authors write that smokers are almost twice as likely to get very sick from COVID-19. Smokers have damaged lungs, so it’s much harder for the body to handle the typical COVID-19 lung infections.
- Immunocompromised individuals
People with weakened immune systems will have a more difficult time fighting COVID-19. They may also not respond as well to vaccines, so they are more prone to re-infection. This includes:- Individuals receiving cancer treatment, such as chemotherapy
- Individuals who take immunosuppressive medications for other conditions
- People with advanced HIV
- Organ or stem cell transplant recipients
- Pregnancy
According to the Mayo Clinic, pregnant people catch COVID-19 at the same rate as people who aren’t pregnant. However, pregnancy does raise the risk factor for developing severe COVID-19, up to at least a month after giving birth.

What can urgent care do for COVID-19?
Urgent care providers can test for COVID, evaluate your condition, and prescribe treatment if needed. Many clinics also offer vaccinations. Urgent care is not appropriate for severe symptoms like trouble breathing, chest pain, or confusion. If you have these symptoms, go to the ER.
Here’s how urgent care can help you manage COVID-19:
- Symptom management
Urgent care providers can examine you and offer advice on managing symptoms like fever, sore throat, or cough. They may recommend over-the-counter medications, prescribe other treatments, share hydration strategies, and provide rest plans to help you recover at home. If you have other health conditions, they can adjust recommendations accordingly.
- COVID-19 diagnostic tests (PCR and rapid antigen)
Most urgent care centers offer both rapid antigen tests and PCR tests. Rapid tests give results in under an hour, while PCR tests are more accurate but take longer. Testing is useful if you’re unsure whether your symptoms are COVID-19 or something else.
- Prescribe medications
If you test positive and meet the eligibility criteria, providers at many urgent care centers can prescribe antiviral medications such as Paxlovid. These treatments work best when you take them within five days of symptoms starting.
- Monitoring for complications/symptom progression
Urgent care can evaluate critical signs like oxygen levels, lung condition, heart rate, and more. If your symptoms worsen, they can decide whether you need to go to the emergency room.
- Offer a vaccination
Many urgent care clinics offer COVID-19 vaccines. It’s best to call ahead and check that your local clinic has the vaccine available. (Get answers to your COVID-19 vaccine questions.)
- Current guidance on when to isolate
According to Dr. Ashley Kelley, a physician at Included Health, “Earlier during the COVID pandemic, it was recommended to isolate for 5-10 days, but current guidance is much more liberal.” According to the CDC, “The updated Respiratory Virus Guidance recommends that people stay home and away from others until at least 24 hours after both their symptoms are getting better overall, and they have not had a fever (and are not using fever-reducing medication).” Dr. Ashley Kelly states, “Note that this is not just for COVID but for colds, flus and all types of respiratory illnesses. We used to treat COVID differently and require longer isolation than other illnesses, but that guidance has changed. Now we treat it like any other respiratory illness, and we recommend staying home until you are feeling better, not only to help you recover but also to prevent the spread of your illness to others. If you must go out in public and aren’t feeling at your best, masks are still useful to prevent the spread of your illness.”
What to expect from a COVID-19 test at an urgent care
During a COVID-19 test, a provider will swab your nose to collect a sample. It’s mildly uncomfortable, but it lasts only a few seconds. Some results come in 15 minutes, while others take a few days. Your provider will tell you when and how you’ll receive results.
COVID-19 tests are a quick, routine part of urgent care visits. A healthcare provider will use a long swab, similar to a long Q-tip, to collect a sample from your nose. This process may feel mildly uncomfortable, and many patients describe brief sensations like stinging or tickling.
Urgent care clinics typically offer two types of tests: rapid antigen and PCR. Rapid tests provide results within 15–30 minutes, whereas PCR tests take 1-3 days. Most clinics will call or message you with PCR results, while providers will share rapid results in the same visit.
Types of COVID tests available at urgent care
Most urgent care clinics offer rapid antigen, PCR, and antibody tests, but only PCR and antigen tests can diagnose a current infection. Rapid tests give results in minutes but may miss early infections. PCR results take a few days, but are very accurate.
To diagnose a current case of COVID-19, there are two major types of tests: an antigen test and a PCR test. Urgent care providers will decide which test to use based on your symptoms, exposure risk, timing of illness, and how quickly you need results. In some cases, they might perform both tests.
Here are the details about each test:
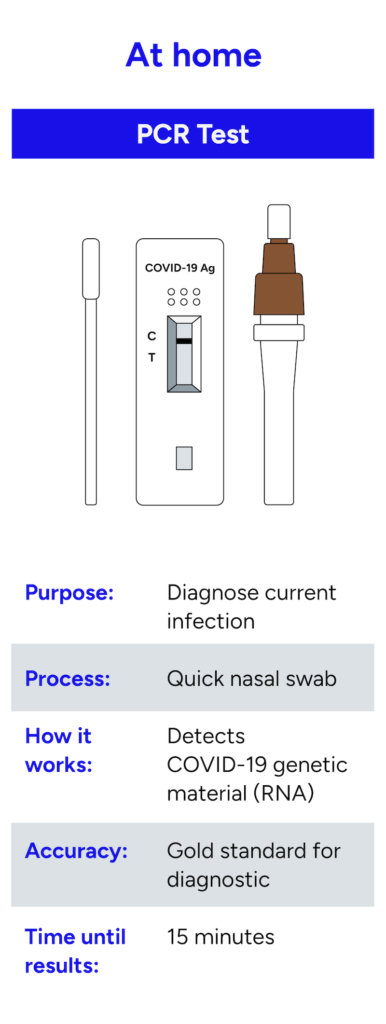
- PCR Test (Polymerase Chain Reaction)
- How it works: A healthcare provider collects a sample with a nasal swab and sends it to a lab. The lab uses a process called polymerase chain reaction to amplify and detect whether the nasal sample contains the virus’s genetic material (RNA). Even tiny amounts of viruses can trigger positive results.
- Speed: Most results come back in one to three days, depending on the lab and local demand.
- Pros: PCR tests are the gold standard in terms of accuracy. They can detect COVID-19 even in people with very low virus levels, including early in the infection or after symptoms start to fade.
- Cons: You need to wait a few days for results, which can delay treatment or decisions about isolating. PCR tests are only available in clinics.
- Best for: Confirming infection, especially in symptomatic or high-risk patients.
- How it works: A healthcare provider collects a sample with a nasal swab and sends it to a lab. The lab uses a process called polymerase chain reaction to amplify and detect whether the nasal sample contains the virus’s genetic material (RNA). Even tiny amounts of viruses can trigger positive results.
- Rapid Antigen Test
- How it works: A healthcare provider collects a nasal swab, mixes it with a liquid solution, and applies the mixture to a test strip. The strip detects proteins (antigens) that coat the surface of the COVID-19 virus. If the proteins are present, the strip produces a colored line to indicate a positive result.
- Speed: Most results come back in one to three days, depending on the lab and local demand.
- Pros: PCR tests are the gold standard in terms of accuracy. They can detect COVID-19 even in people with very low virus levels, including early in the infection or after symptoms start to fade.
- Cons: You need to wait a few days for results, which can delay treatment or decisions about isolating. PCR tests are only available in clinics.
- Best for: Quick checks when time matters more than precision.
- How it works: A healthcare provider collects a nasal swab, mixes it with a liquid solution, and applies the mixture to a test strip. The strip detects proteins (antigens) that coat the surface of the COVID-19 virus. If the proteins are present, the strip produces a colored line to indicate a positive result.
Antibody tests can show if you had COVID-19 in the past, but they don’t detect current infections or guide treatment decisions. A positive result suggests you had the virus at some point.
Here’s more information about the antibody test:
- Antibody test
- How it works: A healthcare provider draws a blood sample and sends it to a lab. The lab checks to see if your blood contains COVID-19 antibodies, which are proteins your immune system makes after you’ve been infected. A positive result suggests you had COVID-19 in the past and your body produced an immune response.
- Speed: Most test results come back in one to three days.
- Pros: Antibody tests can help confirm whether you had COVID-19 in the past, even if you didn’t notice symptoms. Some people use them to understand their exposure history or to contribute to research.
- Cons: These tests don’t detect active infection. You can’t use them to confirm whether you currently have COVID-19 or to make decisions about isolation or treatment.
- Best for: Checking for past infection.
- How it works: A healthcare provider draws a blood sample and sends it to a lab. The lab checks to see if your blood contains COVID-19 antibodies, which are proteins your immune system makes after you’ve been infected. A positive result suggests you had COVID-19 in the past and your body produced an immune response.
Home treatments for mild COVID symptom management
You can manage mild COVID-19 symptoms at home with rest, fluids, and over-the-counter medications like ibuprofen for fever and body aches. Monitor your symptoms closely, stay isolated, and contact your doctor if your symptoms get worse.
If you’re recovering at home with mild COVID-19 symptoms, here are some ways to manage your symptoms:
Dr. Kelley reminds us that home remedies can be effective for patients with COVID-19, but you need to be cautious, especially when taking anything over the counter. “While there are no over-the-counter medications that can cure COVID-19, there are several home remedies and symptom management strategies that can help you feel better during your recovery. The key is to treat the symptoms you’re experiencing.
For example, medications like Tylenol (acetaminophen) or Ibuprofen can help reduce fever and relieve body aches. Cough suppressants may ease a persistent cough, and decongestants can provide relief from nasal or chest congestion. Additionally, vitamins and minerals such as vitamin C, vitamin D, and zinc may help support your immune system. However, it’s important to note that while these supplements can help prevent illness, they do not cure COVID-19 or speed up recovery. If you choose to take vitamins, be sure to follow recommended dosages—excessive amounts can be harmful, especially for those with chronic health conditions.
Rest is another critical component of recovery that is often overlooked. Fatigue is one of the most common symptoms of COVID-19 and is your body’s signal that it needs rest. This doesn’t necessarily mean staying in bed all day, but rather listening to your body’s needs. If you’re feeling tired, allow yourself to sleep and relax. When you start to feel more energetic, gentle movement and walking around can be beneficial. In fact, some severe COVID-related complications, such as pneumonia or blood clots—can result from prolonged immobility. Striking a balance between adequate rest and light movement, based on how you feel, is essential for a healthy recovery.”
How Doctor On Demand can assist with COVID-19
Doctor On Demand offers virtual urgent care visits with board-certified providers who can help you manage COVID-19. If you have symptoms or recently tested positive, you can speak with a doctor to get answers, discuss treatment options, and decide if you need in-person care.
A Doctor On Demand urgent care visit can connect you with a doctor in as little as five minutes. Your doctor can review your symptoms, walk you through home care, recommend over-the-counter medications, and prescribe antivirals such as Paxlovid if you’re eligible. They can also answer questions about when to seek in-person care and how to protect others around you.If you’re unsure what to do next, a Doctor On Demand COVID-19 visit gives you quick, convenient access to expert medical advice — without ever leaving the house.
How to prepare for your Doctor On Demand visit
To get the most out of your virtual Doctor On Demand COVID-19 visit, find a quiet, well-lit space with a strong internet connection. Write down key details like your symptoms, any recent tests, and questions you want to ask, so nothing gets missed.
A little prep beforehand will help your Doctor On Demand provider assess your situation accurately and recommend the best next steps.
Here’s how to prepare for your virtual Doctor On Demand visit:
- Charge your device and check your setup.
Make sure your phone, tablet, or computer is fully charged or plugged in. Test your camera, microphone, and speakers ahead of time to avoid last-minute tech issues.
- Pick a quiet, well-lit space.
Sit somewhere with good lighting so your doctor can see you clearly during the video call. It’s best to be in a private space where your visit won’t be interrupted.
- Write down your symptoms
Include when they started, how severe they are, and whether they’re getting better or worse. This helps your doctor spot patterns and decide if you need further care or medication.
- Note any recent COVID-19 tests and vaccinations
If you’ve already taken a rapid or PCR test, jot down the type, date, and result, even if it was negative. Your doctor may use this to guide diagnosis or treatment.
- Prepare your questions
Think about what you want to know before the call. For example: Should I isolate? Can I take Paxlovid? When should I go to urgent care or the ER? If you have any chronic or underlying medical conditions, mention them to your doctor.
- Keep your photo ID nearby
Some visits may require identity verification, especially if you’re getting a prescription.
Doctor-answered COVID-19 FAQs
Doctors answer common questions about COVID-19, including symptoms, testing, and how urgent care clinics can help. Learn what to watch for, how tests work, and what to expect if you need care.
- Can you go into an urgent care clinic with COVID-19?
Yes, most urgent care clinics will accept patients with COVID-19. Before you enter, let the front desk know so they can take proper precautions. Sometimes, they may ask you to wait in your car or use a different entrance.
- Can you get a COVID-19 test at urgent care?
Yes, most urgent care clinics offer both rapid antigen and PCR COVID-19 tests. A provider will choose the right test based on your symptoms and timing, and whether you need quick results.
- How long does a COVID-19 test take at urgent care?
The actual nasal swab process only takes a few seconds, but your total visit time depends on the clinic’s demand that day. Rapid tests give results in about 15 minutes. PCR test results usually take one to three days, depending on the lab.
- Does urgent care do rapid COVID-19 testing?
Yes, many urgent care centers offer rapid antigen tests. During the test, a provider will use a nasal swab to collect a sample. They’ll share the results in the same visit, usually within 15 minutes.
- Are COVID-19 tests still free at urgent care?
The cost of a COVID-19 test depends on your insurance and the clinic. Some insurance plans still cover testing, but not all. If you’re uninsured, you may need to pay out of pocket. Some clinics offer free testing, so call ahead to ask about costs.
- Can urgent care test for other illnesses that have the same symptoms as COVID-19?
Yes, urgent care providers can test for flu, strep throat, RSV (respiratory syncytial virus), and other illnesses that cause similar symptoms to COVID-19. They may run multiple tests during the same visit to help figure out what’s causing your symptoms and how to treat them.
- Can you get the COVID-19 vaccine at urgent care?
Many urgent care centers offer COVID-19 vaccines, but the availability depends on the clinic. It’s best to check the clinic’s website or call ahead to ask whether they have vaccines in stock and if you need an appointment.
- Can urgent care doctors prescribe COVID-19 medication?
Yes, urgent care doctors can prescribe a COVID-19 medication such as Paxlovid if they feel you need it. They’ll review your symptoms, health history, and test results to decide if treatment is appropriate.
- Can urgent care prescribe COVID-19 antivirals?
Yes, urgent care doctors can prescribe antivirals like Paxlovid if you test positive and meet the eligibility guidelines. These medications work best if you start them within five days of developing symptoms.
- Do urgent care clinics provide a doctor’s note for work or school?
Yes, many urgent care doctors can provide a doctor’s note that includes your COVID-19 diagnosis and how long you should stay home before returning to work or school.
About the authors

Dr. Heather Hockenberry is board certified in family medicine. She earned her doctor of medicine degree at the University of Nevada Reno School of Medicine where she also completed her internship and residency in family medicine, serving as chief resident during her time there. As an urgent care physician for a decade prior to coming to Included Health, she treated acute illnesses and injuries of a diverse nature in a clinic setting. She came to Included Health in 2015 as a staff physician, and currently serves as an associate medical director supporting our clients from a clinical perspective.

Quan Lam is a copywriter with over 15 years of experience writing and editing content for both start-ups and legacy brands, as well as 2 years of writing experience exclusively within the healthcare space. She currently lives and works in New York City.



