A sinus infection can be a minor or major problem, depending on your symptoms and situation. Learn when to see a doctor, when to go to the ER, and when telehealth or at-home care may be enough. Also, see what your treatments might include.
When to go to the ER for a sinus infection
Head to the ER right away if you have a sinus infection that includes new vision problems, significant swelling around your eyes, a severe headache, confusion, or trouble speaking. These symptoms suggest the infection may be spreading and should be treated as an emergency.
Other signs that need urgent attention include double vision, eye pain, a bulging eye, a stiff neck, or a high fever. If you’re struggling to breathe or your thinking feels off and lethargic, don’t wait. Go to the ER immediately. Any neurological changes, like slurred speech, coordination issues or difficulty walking and seizures are red flags to call 911.
The vast majority of sinus infections aren’t life-threatening, but some can be. Rare complications include meningitis (an infection in the brain’s lining), brain abscesses, or sepsis. You’re more at risk if you have chronic sinusitis, cystic fibrosis, nasal polyps, a deviated septum, asthma, or a weakened immune system.
According to a 2012 study titled “IDSA Clinical Practice Guideline for Acute Bacterial Rhinosinusitis in Children and Adults” from the Infectious Diseases Society of America (IDSA), you might need more aggressive care if your infection isn’t improving after treatment. That could mean imaging tests or a referral to a specialist. If you’re not getting better within a few days of treatment, don’t wait—seek medical help.
When to go to urgent care for a sinus infection
Urgent care is a good option when your sinus infection symptoms are too uncomfortable to wait, but not dangerous enough for the ER. If your sinus symptoms have lasted more than 7–10 days or worsened after getting better, urgent care can help.
Watch for facial pain, pressure, post-nasal drip, or thick mucus that won’t go away. You might also have fatigue, sore throat, fever, or jaw pain. A toothache or earache tied to sinus pressure could mean the infection is spreading deeper.
Not sure if it’s a cold, allergies, or a sinus infection? Urgent care providers can help figure that out, too.
When to use telehealth for a sinus infection
Mild or moderate sinus issues are often manageable through telehealth, especially if you don’t have red-flag symptoms. In a virtual visit, you can talk to a provider about common symptoms like nasal congestion or discolored nasal discharge, a dull headache, fatigue, bad breath, or mild facial pressure.
Your doctor can help figure out whether it’s a viral sinus infection or a bacterial one, and recommend what to do next. They can also prescribe medications like antibiotics, steroid nasal sprays, or antihistamines if allergies are involved, and refer you to an ENT specialist if your symptoms don’t improve.
Telehealth is especially helpful if you have allergies (hay fever), GERD (acid reflux that irritates the throat and sinuses), or chronic conditions like cystic fibrosis that may be making your symptoms worse.
Follow-up visits can also be done virtually, making it easier to track progress without needing to visit a clinic.
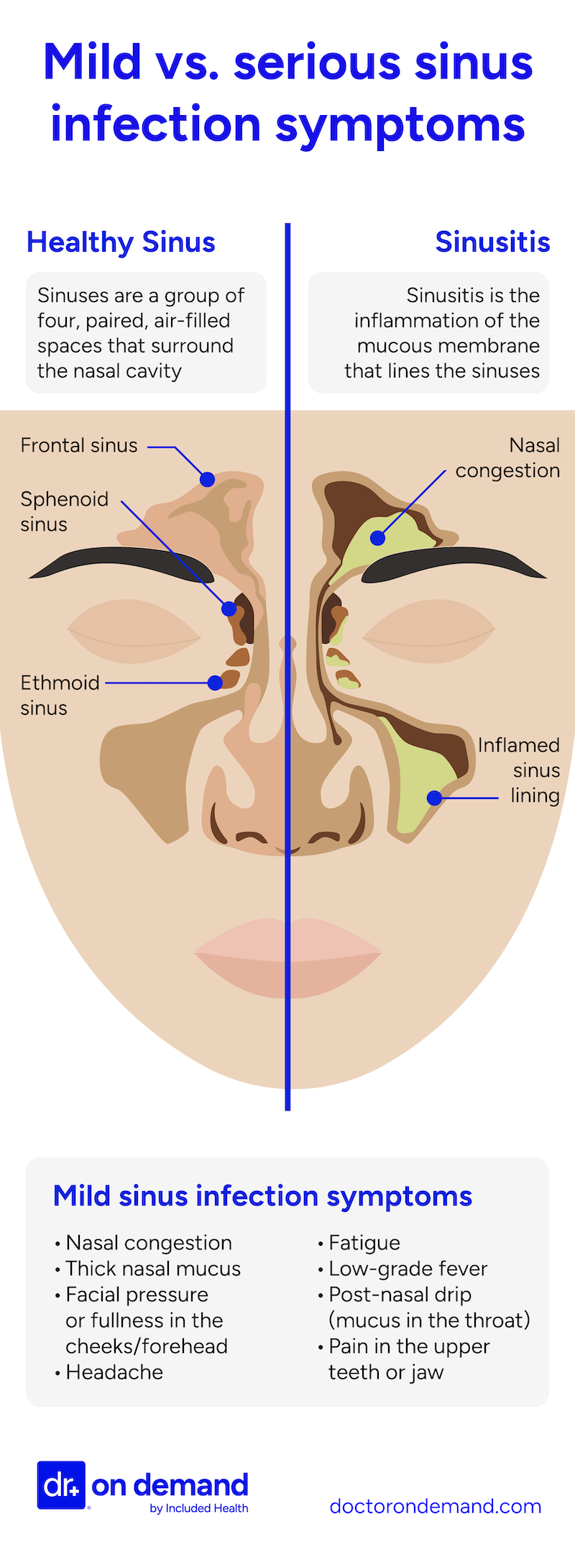
Mild vs. serious sinus infection symptoms
Most sinus infections are mild and clear up within 7–10 days. But in rare cases, the infection can become serious, especially if symptoms escalate, last longer than expected, or affect your eyes, brain, or nervous system.
Typical symptoms include congestion, facial pressure, thick mucus, headache, and fatigue. These usually improve with rest, fluids, and over-the-counter medications.
Serious symptoms are much less common, but they can include swelling around the eyes, vision changes, high fever, confusion, trouble walking or talking. These signs may point to a spreading infection and need immediate medical attention.
Use the chart below to tell the difference, and don’t ignore symptoms that feel extreme or out of proportion for a sinus infection.
A 2020 review titled “Current and Future Treatments of Rhinitis and Sinusitis” in The Journal of Allergy and Clinical Immunology: In Practice explains that sinus infections vary widely in cause, severity, and treatment response. Researchers emphasize that a better understanding of different subtypes, especially chronic or recurrent cases, is leading to more tailored and effective care.
What can a hospital ER do for a sinus infection
The majority of sinus infections do not require ER or hospital care. However, If your sinus infection becomes dangerous, the emergency room is equipped to handle it. ER doctors are trained to look for serious problems, such as a brain abscess, orbital cellulitis (an infection around the eye), or a rapidly progressing fungal sinus infection.
They may order a CT or MRI scan immediately if they suspect any of these. These tests show whether the infection has spread deeper into your head. They may also do bloodwork to evaluate blood counts and inflammatory markers. Treatment can begin immediately if necessary.
You may also get IV antibiotics on the spot. These are often stronger and faster-acting than pills and are used when the infection is severe or spreading quickly. If you’re dehydrated or running a high fever, they may also give you IV fluids. This will help keep your body stabilize while it fights off your infection.
ER staff also work to ease your symptoms as soon as possible. Depending on what you’re experiencing, they may:
- Bring down a high fever: If you have a strong fever when you arrive, they’ll give you medicine like acetaminophen or ibuprofen to lower it. This helps reduce strain on your body and makes you feel better faster.
- Manage your pain: Sinus infections can cause sharp headaches and painful pressure in your face. You may be offered stronger pain relievers than what’s available over the counter if your pain is severe and not responding to home remedies.
- Help you breathe more easily: If swelling in your sinuses makes it hard to breathe or causes constant coughing from postnasal drip, they might use nasal sprays or breathing treatments to open your airways and reduce congestion.
- Call in a specialist if needed: ENT doctors can look at blocked sinuses or ear issues. A neurologist might step in if you’re confused or have a severe headache. If the infection seems rare or unusually stubborn, an infectious disease expert could be consulted right there in the ER.
The ER can provide rapid diagnostics and aggressive treatment measures that aren’t available in an outpatient setting, which can be lifesaving if a sinus infection has led to complications like a brain infection or sepsis.
When is sinus pressure dangerous
Sinus pressure is a common symptom of sinus infections and even ordinary colds. You’ll typically feel it in your forehead, cheeks, or around the eyes due to congestion in those sinus cavities. By itself, sinus pressure (even when painful) is usually not dangerous. It’s a typical part of sinusitis.
That said, there are times when sinus pressure really should not be ignored. It becomes more concerning if the pressure is severe and localized (think extreme pain on only one side of your face), or if it’s accompanied by any of the red-flag symptoms mentioned earlier (think vision changes or swelling around the eye).
Go see a doctor immediately if you have:
- A high fever (over ~102°F or 39°C)
- A stiff neck or difficulty moving your neck
- An unusually severe headache
- Mental confusion or extreme drowsiness
These are signs the infection may be spreading beyond your sinuses.
For instance, pressure plus eye swelling could mean an infection in the eye socket, and pressure plus neck stiffness or confusion could mean meningitis. However, these situations are very rare.
How to tell if a sinus infection has spread
It’s rare, but a sinus infection can spread by either eroding through bone or traveling through blood vessels. Warning signs of a sinus infection spreading into the central nervous system often overlap with sudden vision problems, a persistent high fever, severe headaches, or a very stiff neck.
You might also notice changes in your mental state, such as personality changes, increased confusion, or difficulty concentrating. In advanced cases, there may be balance issues, trouble with coordination, or even seizures.
Keep in mind that certain people are at higher risk for this kind of complication. If you have chronic sinusitis, cystic fibrosis, or an immune disorder that makes it harder to fight infections, your risk of an infection reaching the central nervous system is higher than the average person.
If any of these symptoms are noticed, you should seek medical care immediately.
The good news is that such complications are very uncommon, but knowing the signs can save your life.
High-risk groups for getting more serious sinus infections
People with underlying medical conditions that affect the immune system, airway structure, or sinus drainage are at higher risk for serious sinus infections. These individuals may develop more frequent infections, longer-lasting symptoms, or complications like eye or brain involvement, especially if not treated early.
“Certain medical conditions can significantly increase the risk of developing severe or chronic sinus infections,” explains Dr. Kurt Gilbert, an Internal Medicine physician with over 11 years of experience. “For example, individuals with asthma or allergies often experience persistent inflammation that disrupts normal sinus drainage, creating an environment where infections can thrive. Similarly, conditions like nasal polyps, a deviated septum, or immune system disorders can impair the body’s ability to clear mucus or fight off infections, leading to more frequent or complicated cases of sinusitis. Early recognition and tailored treatment are crucial for managing these higher-risk patients and preventing potential serious complications.”
You’re more likely to face complications if you have:
- Asthma: Chronic inflammation in the lower airways may increase inflammation in the upper airways, making infections harder to resolve. Studies show that people with asthma and sinusitis together often experience more severe symptoms and more frequent flare-ups.
- Allergies: Allergic rhinitis causes persistent swelling in the nasal passages, which can block normal sinus drainage and create a breeding ground for bacteria. Poorly controlled allergies often lead to recurring or prolonged sinus infections.
- Nasal polyps: These noncancerous growths in the nasal or sinus lining can obstruct airflow and prevent mucus from draining properly. People with nasal polyps often have chronic or severe sinusitis that requires specialized treatment, sometimes including surgery or biologic medication.
- A deviated nasal septum: When the cartilage dividing your nasal passages is off-center, it can block drainage on one or both sides. This increases the risk of mucus buildup and bacterial overgrowth, leading to more stubborn infections.
- GERD (Gastroesophageal reflux disease): Acid reflux can irritate the back of the throat and nasal passages, causing inflammation that mimics or worsens sinusitis. In some patients, untreated GERD may contribute to chronic post-nasal drip and sinus symptoms.
- Cystic fibrosis: This genetic condition causes thick, sticky mucus throughout the body, including the sinuses. People with cystic fibrosis often develop chronic bacterial sinus infections that are difficult to treat and may require aggressive or long-term therapies.
- An immune system disorder: Conditions like HIV, leukemia, uncontrolled diabetes, or the use of immunosuppressive drugs (including chemotherapy or high-dose steroids) reduce the body’s ability to fight off infections. In these cases, sinus infections may spread more quickly or become severe without early intervention.
In addition, dental infections, especially those involving upper molars, can spread into the maxillary sinuses through the surrounding bone. If you have a persistent toothache on one side of your upper jaw along with sinus symptoms like facial pressure or fever, the root cause may be a dental abscess. In those cases, seeing a dentist is essential, as treating the tooth may be the only way to clear the sinus infection.
How to tell the difference between a sinus infection, cold, allergies and COVID-19
Sinus infections usually come with a specific mix of symptoms. You might feel pain or pressure in your face, especially around your cheeks or forehead. Your nose may be stuffed up, and the mucus can be thick and yellow or green, but this doesn’t always mean it’s bacterial. Some people also run a low-grade fever.
Colds are different. They often start with sneezing and a runny nose. You might get a sore throat and feel a little run-down, but the symptoms tend to be milder and go away faster than with a sinus infection.
Allergies (like hay fever) don’t cause a fever. Instead, you’ll likely have clear nasal drainage, itchy or watery eyes, and post-nasal drip. These symptoms often show up in certain seasons or around triggers like pollen, dust, or pet dander.
COVID-19 affects more than just your sinuses. It can cause fever, a dry cough, fatigue, and often a sudden loss of taste or smell. It usually comes with a full-body feeling of illness, not just head or nasal symptoms.
| Symptom | Sinusitis | Cold | Allergies | COVID-19 |
| Facial pressure/pain | Yes | Sometimes | Sometimes | Sometimes |
| Duration of Illness | Over 10–14 days | Under 10 days | Varies | Varies (often 1–2 weeks) |
| Nasal Discharge | Thick, yellow-green (though it doesn’t always mean a bacterial infection) | Thick, whitish or thin | Clear, thin, watery | Sometimes clear or none |
| Fever | Sometimes | Sometimes | No | Yes |
| Headache | Sometimes | Sometimes | Sometimes | Yes |
| Pain in Upper Teeth | Sometimes | No | No | No |
| Bad Breath | Sometimes | No | No | No |
| Coughing | Sometimes | Yes | Sometimes | Yes |
| Nasal Congestion | Yes | Yes | Sometimes | Sometimes |
| Sneezing | No | Yes | Sometimes | Rare |
Home treatments for sinus infections until you see a doctor
Most mild sinus infections get better on their own. At home, you can ease symptoms by staying hydrated, using nasal saline rinses, managing pain with over-the-counter meds, and supporting drainage with rest and warm compresses. These steps often help you recover without needing antibiotics.
“Most sinus infections are caused by viruses or allergies and typically do not require immediate evaluation or antibiotics,” says Dr. Kurt Gilbert, an Internal Medicine physician who has been practicing for over 11 years. “In my experience, infections lasting less than 6-7 days are often viral or related to allergies and can be effectively managed at home with supportive care like hydration, nasal rinses, and rest. However, if symptoms persist beyond this timeframe or worsen, it may be time to seek evaluation.”
If your sinus infection is mild or you’re waiting to see a doctor, there are several simple steps you can take to feel better. Start with rest and hydration. Drinking plenty of fluids helps thin mucus so it drains more easily, and resting gives your body a better chance to fight the infection.
Nasal saline rinses or sprays can also help clear out mucus and reduce congestion. Many people find relief by applying warm compresses over the cheeks, forehead, or bridge of the nose. The warmth may help relax and open your sinus passages, making it easier for fluid to drain.
Over-the-counter medications can reduce discomfort while your body heals. Ibuprofen or acetaminophen can help with facial pain, sinus pressure, or fever. Short-term use of decongestant nasal sprays or oral decongestants may shrink swollen nasal passages, but these decongestant medications shouldn’t be used for more than 3 days in a row and should be avoided in folks that have uncontrolled hypertension. If your symptoms are tied to allergies, a steroid nasal spray or antihistamine may help reduce inflammation and improve airflow.
Try to stay upright during the day and elevate your head while resting. Lying flat can make congestion worse and slow drainage.
Most viral sinus infections start to improve within a week. If your symptoms last more than 10 days, get worse after briefly improving, or feel unusually intense, contact your doctor. You may need antibiotics or a referral to an ear, nose, and throat (ENT) specialist.
How Doctor On Demand can assist with sinus infections
Doctor On Demand makes it easy to get help without leaving home. Their board-certified physicians can evaluate your sinus infection symptoms, offer treatment options, and prescribe medications if needed. For example, if your doctor thinks you have a bacterial sinus infection, they can electronically prescribe an appropriate antibiotic. If it appears to be viral or related to allergies, they might suggest supportive care like decongestants, nasal corticosteroids, or antihistamines, which you can get over the counter or via prescription.
They can also help you figure out if in-person care is necessary. Based on your video exam and history, they might reassure you that it’s okay to continue home treatment, or they may advise you to go to urgent care or the ER if they see any red-flag signs.
How to prepare for your Doctor On Demand visit for your sinus infection
Take a few minutes to get organized before your telehealth visit. A little prep goes a long way. It helps your doctor understand what’s going on and speeds up the call.
Here’s what to have on hand:
- List your symptoms. Write down what you’re feeling, when it started, and whether it’s getting better or worse. Even small changes are worth noting.
- Check your temperature. Know your latest reading, and be ready to share any treatments you’ve already tried, such as ibuprofen, decongestants, or saline rinses.
- Share your history. Let the doctor know if you’ve had sinus infections before, or if you’ve got things like a deviated septum or nasal polyps.
- Grab a light. A phone flashlight or small lamp can help the doctor check your nasal passages if needed.
- Set up your space. Choose a quiet, well-lit room with a strong internet connection so nothing gets in the way of your visit.
By being prepared, you’ll help your telehealth doctor accurately assess your condition. They can then give you clear guidance, whether that’s calling in a prescription, suggesting continued home care, or advising an in-person follow-up. And after the visit, you can schedule virtual follow-ups as needed to update the doctor on your progress, all from the comfort of home.
Doctor-answered sinus infection FAQs
Sinus infections typically improve within a week, especially if caused by a virus. Most clear up in about 7 to 10 days. If your symptoms stick around longer or get worse after starting to improve, a bacterial infection could be to blame and antibiotics might be necessary.
The sinus infection itself usually isn’t. But the virus that started it, like the cold or flu virus, can spread to other people. So, if someone catches your virus, they may also develop a sinus infection. Bacterial sinus infections, however, don’t typically spread from person to person.
You may have a sinus infection if you’ve had congestion, facial pressure, and thick yellow or green mucus for more than a week. Worsening symptoms after initial improvement, or pain behind your eyes or upper teeth, are also red flags that suggest a sinus infection, not just a cold.
A sinus infection becomes serious when symptoms include high fever, eye swelling, vision problems, confusion, or stiff neck. These rare signs may mean the infection is spreading to the brain, eyes, or bloodstream, and you may have a medical emergency that needs immediate treatment.
You may need antibiotics if your symptoms last more than 10 days without improving, if they get worse after getting better, or if they start out severe like high fever and facial pain. Your doctor can help you decide.
Yes, but it’s rare. You may need hospitalization if a sinus infection spreads and causes serious complications like meningitis, an eye infection, or a brain abscess, especially in people with weak immune systems. Sudden vision changes, confusion, or a stiff neck are red flags.
Hospital stays for sinus infections vary. A mild case may mean a short stay, but serious complications like a brain infection can require IV antibiotics, imaging, and monitoring for several days or even weeks.
Yes, absolutely. Most do. A viral sinus infection, the most common type, usually clears up on its own in one to two weeks. You don’t need antibiotics unless your doctor thinks it’s bacterial or you’re not improving. Rest, fluids, nasal rinses, and over-the-counter meds can help you fight it off.
You can usually return to work after a sinus infection once your fever has subsided and you feel well enough. If you’re on antibiotics, wait 24 to 48 hours after starting treatment. Stay home longer if you’re still contagious or too run down to function.
A cold may develop into a sinus infection if symptoms persist for more than 10 days or worsen after initially improving. Lingering congestion, facial pain, and thick mucus are key signs the infection has moved into your sinuses.
About the authors

Dr. Connor Lundy is a board-certified Emergency Medicine physician and healthcare leader with over 15 years of clinical practice and administrative expertise. As an Associate Medical Director at Included Health, Dr. Lundy leverages his extensive experience to advance population health initiatives, enhance access to convenient and preventive care services, and drive healthcare quality improvement.

Dr. Brian Knox is board-certified in Internal Medicine and Pediatrics, and has been overseeing clinical services at Included Health for the past 3 years. Prior to joining IH 6 years ago, Dr. Knox spent 9+ years providing primary care to adults and children. He has expertise in preventive care, primary care for the LGBTQ+ population, as well as the management of patients with difficult-to-control diabetes and hypertension.



