Table of contentIn this article
- When to go to the hospital ER for asthma
- How to assess the severity of an asthma attack
- How do hospitals treat asthma attacks?
- Is it an asthma attack or anaphylaxis?
- What to do during a severe allergic asthma attack
- Asthma emergency plan
- Common triggers of asthma exacerbations
- How Doctor On Demand can assist with your asthma
- Doctor-answered asthma FAQ
Asthma can get serious fast. Are you wheezing, tight in the chest, or struggling to breathe? These aren’t just flare-ups—they’re signs you may need emergency care. Knowing when to go to the hospital could protect your lungs (and your life).
When to go to the hospital ER for asthma
If you’re having trouble breathing and your quick-relief inhaler (like albuterol) isn’t working for you, it’s time to get emergency help. This may be more than a flare-up—it could be a serious asthma attack that needs immediate treatment.
Use your rescue inhaler—2 to 4 puffs every 20 minutes for up to an hour. If you’re still struggling to breathe after that, don’t wait. Go to the ER.
Watch for these warning signs:
- You can’t speak more than a few words without gasping.
- Your lips, face, or nails look blue or gray.
- You feel lightheaded, dizzy, confused, or break into a cold sweat—a potential sign of oxygen deprivation.
- Your chest feels tight and you can’t take a full breath.
- You stop hearing wheezing. This “silent chest” means almost no air is moving.
That last one is especially dangerous. If wheezing stops suddenly, it usually means your airways are nearly closed, not that you’re improving. That’s a sign of respiratory failure. Don’t try to wait it out. If something feels wrong, trust your instincts and get help fast.
Your peak flow meter can also help you decide. If your reading is under 50% of your peak best, even after treatment, go to the hospital. Severe asthma can get worse fast. Don’t wait it out and go get help.
A 2019 study in the International Journal of Pediatric and Adolescent Medicine titled “Management of asthma exacerbation in the emergency departments” notes that the first hour is the optimal treatment time, so it’s important to seek the right clinical treatment quickly if you develop severe asthma symptoms.
When to call 911 for asthma
Call 911 right away if you (or someone else) is in serious trouble from an asthma attack. Fainting, collapsing, or being unable to speak all constitute an emergency. Another major warning is what doctors call “silent chest,” when no air movement can be heard at all.
Watch for labored breathing where you or another person is using neck and chest muscles just to take a breath. Hives, swelling of the lips, tongue, or throat (angioedema), or an itchy rash after a known exposure (such as to food, insect stings, or latex) could be a serious allergic reaction known as anaphylaxis. This requires epinephrine, which is not typically used for asthma alone, but is the first-line treatment for anaphylaxis.
If someone becomes unconscious, even briefly, call for help. Paramedics can administer oxygen, albuterol, and/or epinephrine as needed. They’ll also watch breathing patterns and act quickly if oxygen levels drop. These symptoms could become fatal without fast treatment.
When to go to urgent care for asthma
It’s time to head to urgent care if your asthma isn’t improving but you’re not in serious danger, or if you’ve used your rescue inhaler a few times and you’re still wheezing or coughing. You can still walk and talk, but your breathing just isn’t improving.
Check your peak flow meter too. If it’s reading between 50% and 80% of your personal best, you likely need care soon. As long as you’re not turning blue or showing signs of anaphylaxis, urgent care can step in.
Here’s the catch: if your symptoms are getting worse fast, or you have a history of life-threatening asthma like status asthmaticus, go straight to the ER. Urgent care can’t handle severe attacks, and you may be transferred anyway.
When can you use telehealth
Telehealth can be a great option when your asthma is acting up, but not too badly. If you’re coughing more than usual but aren’t short of breath or in distress, a quick virtual visit might be all you need.
Your doctor can refill a prescription, adjust your controller meds, or answer any questions you may have without you having to leave the comfort of home.
It’s also a smart time to check in about your asthma plan. If you have allergic asthma, hay fever, or other allergy symptoms, a telehealth visit can help you identify and manage key triggers, such as dust, pollen, and pet dander.
You and your doctor will talk through your symptoms, review your medications, and walk away with a plan that helps you stay in control of your asthma.
When to wait to see your primary care doctor
Not every asthma flare means a trip to the ER or urgent care. If your symptoms have been mild and steady for several days, it’s usually safe to check in with your regular doctor instead. This is a good opportunity to focus on long-term control.
Are you dealing with seasonal triggers like cold air, mold, or exercise? Are you curious about allergy testing? Are your daily meds not cutting it anymore?
As long as you’re not suffering from too severe chest congestion, and you’re breathing okay and not in the middle of a serious attack, your regular doctor is the right place to start. They know your history and can help put together a sustainable plan.
How to assess the severity of an asthma attack
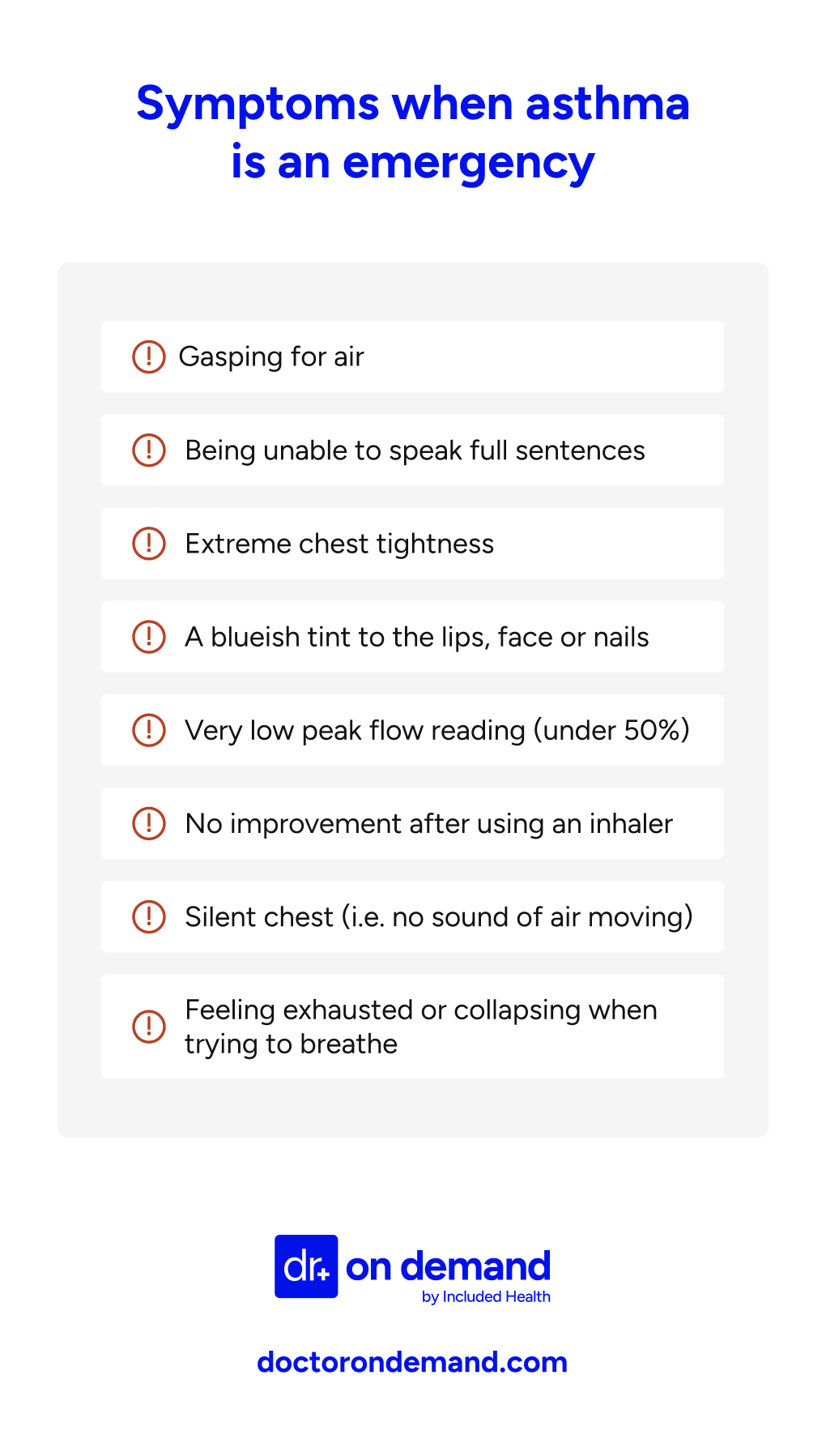
To assess the severity of an asthma attack, watch for signs like struggling to speak, extreme chest tightness, low peak flow, or a blueish tint showing up in your lips or nails. These are symptoms of a serious attack that may need emergency care. Do not wait.
Here are specific signs an asthma attack is serious:
- You’re gasping or you can’t finish a sentence.
- Your chest feels tight.
- You’re using all your energy simply just to breathe.
- Your peak flow reading is low (especially if under 50% of your best).
- Your lips or nails are developing a slightly blueish tint.
- You’ve used your inhaler several times and still aren’t feeling better.
- You have to sit or stand leaning forward just to support and help your breathing (tripoding)
If your breathing becomes quiet (“silent chest”), that means very little air is moving. It’s a late and serious warning sign of impending respiratory failure. Get emergency help right away.
How do hospitals treat asthma attacks?
If your asthma becomes severe, clinical care teams at the ER have what’s needed to get you through it. Doctors work quickly to stabilize your breathing, minimize airway swelling, and make sure your oxygen levels stay at safe levels.
Here’s what they can do:
- Administer oxygen to raise low levels quickly.
- Give you nebulized albuterol and ipratropium.
- Put you on IV steroids (like methylprednisolone) to reduce the inflammation.
- Give you magnesium sulfate, usually if things really aren’t improving.
- Give you a shot of epinephrine (typically only in confirmed anaphylaxis or, in rare cases, when severe allergic asthma isn’t responding to other treatments).
- Give you IV fluids. Asthma attacks can lead to dehydration from rapid breathing.
- Monitor your status. Doctors check your oxygen, blood gases, and your response to meds.
- Put you on ventilation. In extreme cases, like for status asthmaticus or brittle asthma, doctors might need to intubate you and use a breathing machine.
Hospital physicians may also treat other symptoms, like nausea, vomiting, or cold sweats, that might come along with severe asthma attacks.
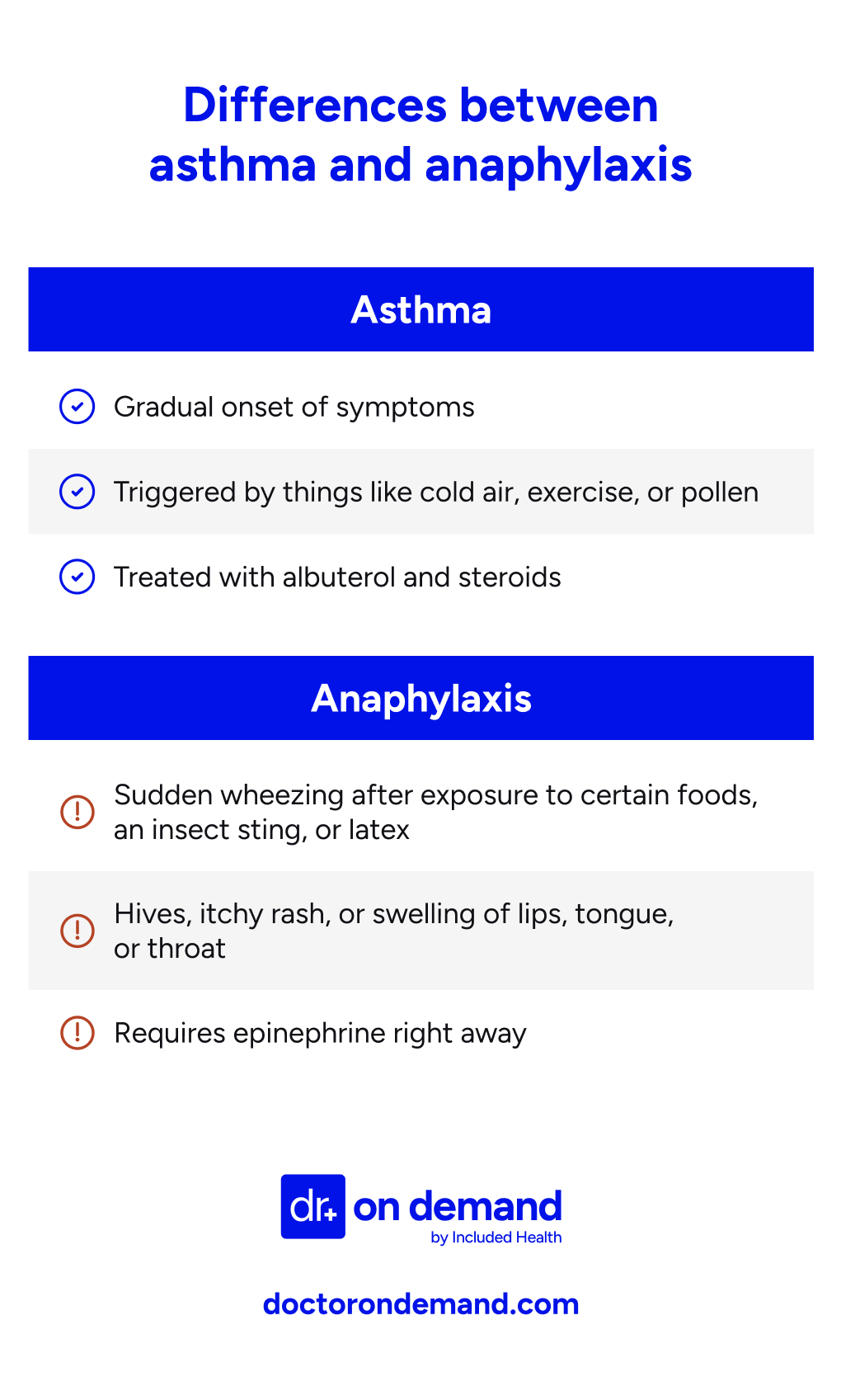
Is it an asthma attack or anaphylaxis?
Asthma and anaphylaxis can look similar. Both can cause wheezing, chest tightness, and trouble breathing. However, they don’t always come from the same trigger and are treated very differently. Asthma tends to build slowly, while anaphylaxis is a rapid and severe bodily reaction to a trigger.
Think back to what just happened. Did your symptoms start right after eating something, getting stung, or touching latex? If you also notice hives, swelling, or an itchy rash, that points to anaphylaxis. You’ll need epinephrine right away.
Asthma, on the other hand, tends to build more slowly. It usually isn’t linked to a sudden trigger like food or a sting.
Asthma and anaphylaxis can still overlap. If you have allergic asthma or other atopic diseases like eczema or allergic rhinitis, it’s possible to experience both asthma and anaphylaxis at the same time. Knowing the signs of each is thus key. But since the two can overlap, it’s safest to treat for anaphylaxis if you’re unsure and if your symptoms include a rash or swelling.
What to do during a severe allergic asthma attack
If you’re having a severe allergic asthma attack, don’t wait it out. Use your reliever inhaler right away. Stay seated upright, breathe steadily, and follow the steps you’ve practiced. If symptoms don’t ease within minutes, then go ahead and call for emergency help.
When using your reliever inhaler (which is usually blue), be sure to take one puff at a time, with 30 to 60 seconds between, and up to 10 puffs total. It’s important during this time to sit up straight, too, since lying down makes breathing harder.
If symptoms continue or you don’t have your inhaler, call emergency services immediately. While waiting, do your best to just stay calm. Steady breathing can help. And if you have a spacer, use it—it improves how the medicine works.
Watch for red flags, too: blue lips, chest tightness, or trouble speaking full sentences. These are signs you need immediate care.
And eventually, even if things settle, follow up with your doctor. A severe attack usually means something in your asthma plan needs adjusting.
What is the 4-4-4 rule for asthma?
The 4-4-4 rule is a simple, lifesaving tool that tells you how to use your inhaler safely during an asthma attack. Take 4 puffs, wait for 4 minutes, and repeat if needed. Symptoms still aren’t improving? Then call emergency services.
You can repeat the 4-4-4 steps every few minutes while you wait for help—up to 20 puffs per hour max. If you have one at hand, you can also use a spacer to make each puff more effective.
However, note that this rule is a safety net rather than a substitute for your asthma action plan. The gist of it? It’s a simple way to act fast when symptoms hit hard.
Asthma emergency plan
An asthma emergency plan is a personalized guide that tells you exactly what to do during a flare-up or crisis, outlining your medications, triggers, warning signs, and when to seek help. The benefit? Having one such plan can make the difference between a controlled event and a medical emergency.
It should be tailored to you: your triggers, your medications, and your health history. Don’t use a one-size-fits-all template. Work with your doctor to build it, and store a copy somewhere easy to find. If your child has asthma, their school or caregiver should have a copy of the asthma emergency plan as well. Dr. Melissa Eirich, MD shares the following Asthma action plans below:
Asthma Action Plan
All asthmatics are different. I have asthma and I understand the struggle with managing daily meds and flares. Because of that, I encourage all of my patients to create an asthma action plan.
Think of it like your personalized roadmap for managing your asthma, both day-to-day and when unexpected symptoms pop up. It’s a step-by-step guide so you know exactly what to do based on how you’re feeling.
The plan uses a simple ‘traffic light’ system: (The Asthma and Allergy Foundation of America has a form you can download.)
- Green Zone (Go!): This is your healthy zone! It lists the daily medications you take to keep your asthma under control and go about your day normally. It’ll also cover what to do for something like exercise-induced asthma.
- Yellow Zone (Caution!): This is when you start to feel a little off—maybe the first signs of a cold, some mild coughing or wheezing, or a tight chest. This part of the plan tells you what extra steps and medications (such as nebulizer treatments or steroids) to take on top of your daily ones, and when to call your doctor.
- Red Zone (Danger!): This is for when your asthma is really acting up, even after you’ve followed the yellow zone steps. We’re talking about hard, fast breathing, trouble speaking, or other serious signs. This section will list critical medications and tell you exactly when to go to the emergency room.
It should also include all your important contact information, your immunization history, your personal best peak flow reading, and list any specific triggers you have.
The beauty of this plan is it takes all the guesswork out of an asthma attack. No more wondering what medication to take or if you need to go to the ER. It’s all laid out for you. And remember, this isn’t set in stone. It’s a ‘living document’ that should be updated, making sure it always fits your current needs. It’s a great tool not just for you, but for your family, caregivers, and even your child’s school.
FYI: How to Use your Inhaler
One of the first things I do with any patient who has been prescribed an inhaler is have them show me how they use it. About 25% of the time, they are not using it appropriately. Sometimes I will show them videos online, but here are the steps:
- Remove the cap and check the mouthpiece to make sure it is clean.
- Shake the inhaler well. If you have a spacer, place it on the mouthpiece.
- Breathe out fully, away from the inhaler.
- Place the mouthpiece in your mouth and close your lips around it.
- As you start to breathe in slowly and deeply, press down on the canister to release one spray.
- Continue to breathe in as slowly and deeply as you can.
- Hold your breath for about 10 seconds, or as long as comfortable.
- Remove the inhaler from your mouth and breathe out slowly.
Acute Asthma Attack: The 4:4:4 Rule
Now, while your personal asthma action plan helps manage your asthma day-to-day, it’s also crucial to know what to do if you have an acute asthma attack (a sudden, severe flare-up). From personal experience with asthma, I know it is frightening to have an acute asthma attack, so knowing what to do helps tremendously.
For those moments, there’s a really helpful first-aid method called the ‘4-4-4 rule’.
Here’s how it works:
First, stay calm and get comfortable, ideally sitting upright. Then, use your quick-relief inhaler (Albuterol):
- Take 4 puffs from your inhaler, using your spacer if you have one.
- After those 4 puffs, wait 4 minutes to see if your breathing improves.
- If you’re still struggling, take 4 more puffs.
- If there’s still no improvement, or if you’re getting worse, it’s time to call emergency services immediately.
This method is all about getting those airways open quickly and effectively during an emergency, buying you time until professional medical help can take over. Knowing this simple sequence can make a huge difference in managing an unexpected attack.
Components of an asthma emergency plan
An asthma emergency plan should include daily medications, steps to take during a flare-up, specific triggers, and emergency contacts. It should also tell you when to seek urgent care, and whom to contact as need be. Having these details written down enables a quick, effective response during an asthma attack.
An asthma emergency plan harbors a few detailed components:
- What you take regularly to control asthma symptoms
- Rescue steps and what to do during a flare-up (e.g. using the 4-4-4 rule)
- What to do if symptoms strike during school, work, or travel
- Known allergens or irritants
- Danger signs and when to seek urgent care
- Emergency contacts
Your asthma emergency plan should be simple, but specific. And keep it written, not just in your head.
Common triggers of asthma exacerbations
Asthma attacks often have a cause—something that sets them off. For you, that might be allergens, a cold, smoke, or even very strong emotions. Knowing your personal triggers helps you stay ahead of flare-ups and out of the ER.
Triggers vary by person, but here are some of the most common ones:
- Colds, the flu, or other respiratory infections
- Allergens, like pollen, dust, mold, or pet dander
- Cockroach droppings (especially in older buildings)
- Smoke — from cigarettes, wildfires, or strong chemicals
- Scented products: perfumes, air fresheners, cleaning sprays
- Breathing in cold air or exercising hard
- Intense emotions like laughing or crying too much
- Certain foods, such as eggs, milk, peanuts, or tree nuts, if you have a food allergy that can trigger anaphylaxis.
- NSAIDs like aspirin or ibuprofen, especially if you have nasal polyps
- Workplace irritants (e.g. metals, wood dusts, cleaning agents, isocyanates, latex, flour)
You don’t have to avoid everything, but knowing what sets you off can help you plan. That might mean keeping your inhaler nearby, using an air filter, or steering clear of certain places or products when you can.
A study titled “Acute asthma, prognosis, and treatment,” published in 2017 in the Journal of Allergy and Clinical Immunology, explains that asthma is a manageable chronic disease that requires patients to clearly understand and avoid its key triggers. A little awareness can go a long way.
How Doctor On Demand can assist with your asthma
Doctor On Demand makes asthma care easier with 24/7 video visits you can do from home. Whether your symptoms are acting up or you just need help managing triggers or medications, licensed providers are ready to guide your next steps—no waiting rooms, no travel.
Not sure if your meds are working? Symptoms getting worse? A Doctor On Demand provider can help you decide what to do next, whether that means adjusting your treatment or heading to urgent care.
They’ll check in on how you’re doing, may prescribe oral steroids or inhalers, and walk you through a plan tailored to your needs. That includes managing allergic asthma or rhinitis, plus practical ways to avoid and handle common allergic triggers like pollen, dust, or air pollution.
How to prepare for your Doctor On Demand visit for asthma
Being prepared helps your Doctor on Demand provider treat you more effectively. Before your appointment, gather a few key details: your peak flow numbers, current medications, recent symptoms, and any known triggers. The more you share, the better your care will be.
Here’s what to have on hand:
- Your peak flow meter and your most recent readings
- A list of meds you’ve used, and what helped or didn’t
- Your inhalers and spacer, close by
- Notes on recent contact with triggers like pets, perfume, or smoke
- Info about any allergic reactions like hives, swelling, or rash
- A full description of your symptoms: coughing, tight chest, trouble breathing, or anything else
Doctor-answered asthma FAQ
Yes. If your rescue inhaler isn’t helping and you’re still struggling to breathe, it’s time to head to the hospital. Doctors there can monitor you closely and give stronger, faster-acting treatments than what you have at home.
Severe asthma needs more than at-home care, In the hospital, you can be put on oxygen, IV steroids, or nebulizer treatments. You’ll also receive around-the-clock attention. This will help stop the attack, prevent complications, and get your breathing back on track.
Most often, hospitals give asthma meds through a nebulizer, which turns medication into a mist you inhale deeply. If you’re stable, you might still use an inhaler with a spacer. For serious symptoms, IV meds are used. In emergencies like status asthmaticus or anaphylaxis, other drugs like magnesium sulfate or epinephrine could be added too.
If someone passes out during an asthma attack, they’ll likely be put on a ventilator with a breathing tube. This keeps oxygen flowing while the team works to open up the airways using powerful medications.
It varies. Some asthma patients return home from the hospital the next day. Others, especially if they have status asthmaticus, might need several days to fully recover.
Doctors watch for key signs like your oxygen levels, breathing rate, and peak flow. They may also check carbon dioxide levels and how well you respond to medications like albuterol and steroids
Red flags include when you can’t speak clearly, your lips or fingers turn blue, or your chest goes quiet (no wheezing—just silence). If your rescue inhaler isn’t working, get to the ER immediately.
It depends. A mild asthma flare might ease up in under an hour, but a more serious one can last for hours or even days if it’s not treated early. In any case, the sooner you act, the faster you’ll recover.
Yes, albuterol is usually the first thing ER doctors give, often through a nebulizer. It’s sometimes combined with ipratropium to boost relief. You may need several doses, depending on how your lungs respond.
If you can’t catch your breath, your skin turns blue, you lose consciousness, or your usual meds stop working, this is a medical emergency. Don’t wait. Get help immediately.
About the authors

Dr. Connor Lundy is a board-certified Emergency Medicine physician and healthcare leader with over 15 years of clinical practice and administrative expertise. As an Associate Medical Director at Included Health, Dr. Lundy leverages his extensive experience to advance population health initiatives, enhance access to convenient and preventive care services, and drive healthcare quality improvement.

Dr. Brian Knox is board-certified in Internal Medicine and Pediatrics, and has been overseeing clinical services at Included Health for the past 3 years. Prior to joining IH 6 years ago, Dr. Knox spent 9+ years providing primary care to adults and children. He has expertise in preventive care, primary care for the LGBTQ+ population, as well as the management of patients with difficult-to-control diabetes and hypertension.



