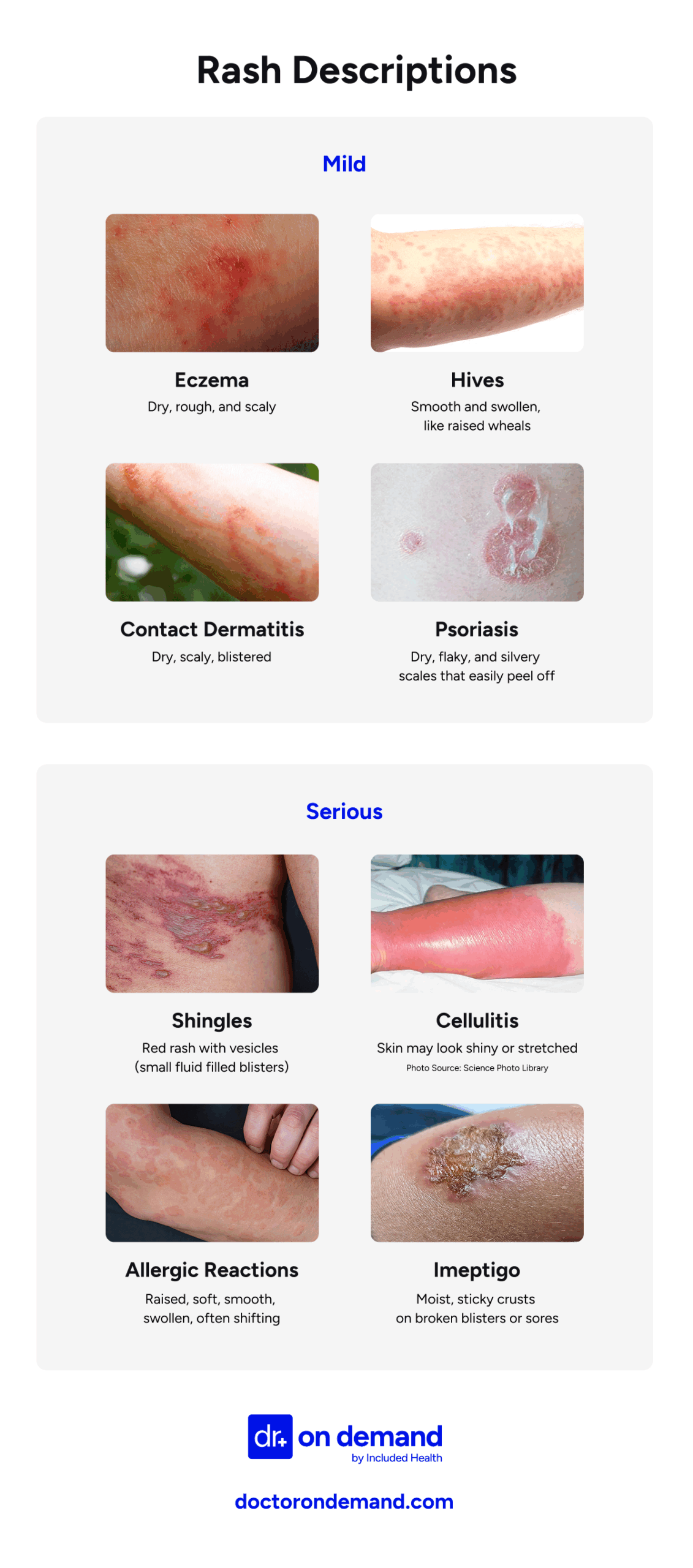
Not sure when a rash needs medical attention? This guide helps you determine whether your rash is best treated at urgent care, an ER, through a telehealth session, or at home. You’ll also find a chart comparing mild and serious skin rashes.
When to go to urgent care for a skin rash
Visit urgent care if your rash worsens, lasts more than a few days, or is accompanied by mild symptoms such as low-grade fever, localized swelling, or itching. Urgent care can handle most uncomplicated rashes, but more serious signs, such as a high fever, blisters, or facial swelling, require emergency care.
Visit urgent care if your rash worsens, lasts more than a few days, or accompanies mild symptoms such as a low-grade fever, swelling, or itching, but without signs of a medical emergency. Urgent care is often the best place to start for new or uncomfortable rashes that don’t appear to be dangerous but still require attention.
When to go to the ER for a skin rash
Go to the emergency room if you have a rash accompanied by a high fever, facial swelling, blisters, confusion, low blood pressure, or rapid spreading of the rash. These symptoms may point to a serious allergic reaction, infection, or immune response — such as Stevens-Johnson syndrome or DRESS — that requires immediate hospital care.
Stevens-Johnson syndrome is a rare drug reaction that causes skin blistering and sores in the eyes, mouth, or genitals. DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) is another delayed medication reaction that can cause rash, fever, facial swelling, and organ inflammation.
Also seek emergency care for rashes with purple or black spots (purpura or necrosis), severe pain, or symptoms such as dizziness, a low pulse, or delirium. These may signal life-threatening conditions such as meningococcemia, sepsis, or necrotizing fasciitis. If you’re immunocompromised and develop a new rash, seek evaluation promptly, even if the symptoms seem mild.
When you can use telehealth for a skin rash
Telehealth is appropriate for mild, localized rashes without fever, swelling, or rapid spread. Conditions like eczema, contact dermatitis, insect bites, or ringworm often respond well to virtual care. But if your rash is painful, worsening, or affects your eyes, mouth, or genitals, you should be seen in person.
Telehealth works best when the rash is easy to photograph and there are no signs of a serious illness. Mild hives, fungal infections, or allergic reactions are commonly diagnosed this way. Providers can often prescribe creams or antihistamines and advise whether in-person care is needed.
According to Brian Knox, MD, the following are appropriate times to use telehealth for a skin rash:
- New, non-severe rashes
- Recurrence of a previous non-emergency rash
- Questions about preventing rashes from recurring
- Hives (without any breathing difficulty)
- Eczema flares
- Mild cellulitis
- Fungal infections (such as ringworm or athlete’s foot)
Avoid telehealth for rashes accompanied by fever, severe pain, facial swelling, or shortness of breath. These may indicate serious conditions, such as infection, drug reactions, or anaphylaxis. Virtual care is also not recommended for new rashes in immunocompromised individuals or rashes that involve mucous membranes (such as the eyes, mouth, or genitals).
When to go to a dermatologist for a skin rash
See a dermatologist if your rash is persistent, keeps coming back, doesn’t improve with standard treatment, or affects sensitive areas, such as the face, eyes, mouth, or genitals. You should also seek specialist care if the cause of your rash is unclear or if it may be related to an autoimmune condition.
Dermatologists have the tools to diagnose rashes that don’t respond to typical therapies and can offer advanced treatments or testing, such as skin biopsies, patch testing, or biologics.
While dermatology care is sometimes limited by location, wait times, or insurance, it plays a crucial role in treating complex or recurring skin conditions. A 2018 study, “The Value of Urgent Care Dermatology,” emphasized that urgent care providers can manage many routine rashes, allowing dermatologists to focus on more serious or urgent conditions that might otherwise overwhelm emergency departments.
Common skin rashes treated at urgent care clinics
Urgent care clinics handle many everyday skin rashes, especially when they appear suddenly or aren’t spreading rapidly. These clinics are often the first stop for new cases of itching, redness, or irritation, and clinics can treat most rashes without you needing to see a specialist right away.
You can usually go to urgent care for:
- Hives – raised, itchy welts often triggered by allergies
- Fungal infections – scaly, ring-shaped rashes like ringworm or athlete’s foot
- Scabies – a rash caused by tiny mites, often between fingers or around the waist
- Insect or flea bites – red, itchy bumps from minor bites or stings
- Mild eczema – dry, itchy patches that flare on the arms, legs, or face
- Contact dermatitis – irritation or rash from skin contact with plants, metals, or soaps
- Heat rash – tiny bumps from trapped sweat, usually in hot or humid weather
- Candida (yeast) infections – red, irritated skin in moist areas like under the breasts or groin
- Intertrigo – raw or inflamed skin in skin folds, often worsened by moisture
- Early drug rashes – red or itchy rashes that appear days after starting a new medication
- Blisters – small fluid-filled bumps, unless widespread or infected
- Small patches of cellulitis – warm, red, painful skin without fever or spreading
- Minor impetigo – honey-colored crusty sores, usually around the nose or mouth
- Perioral dermatitis – red bumps around the mouth, nose, or eyes
- Actinic keratosis – rough, scaly patches from sun damage that may be treated or referred
- Mild rosacea – facial redness or bumps that flare from triggers like heat or alcohol
These conditions often respond to short-term treatments, such as steroid creams, antihistamines, antifungals, or oral medications for infection or inflammation.
Some rashes and related skin conditions need emergency or specialist care instead of urgent care. If your symptoms include a high fever, widespread blisters, facial swelling, or a rash in the eyes, mouth, or genitals, head to the emergency room or contact your primary care provider right away.
Conditions that usually aren’t treated in urgent care include:
- Measles – a contagious viral illness with a full-body rash and fever
- Shingles involving the eye – can threaten vision and requires specialist care
- Widespread drug rashes – especially with fever, blisters, or swelling
- Meningococcemia – a rapidly spreading infection with a purple rash, fever, and confusion
- Necrotizing fasciitis – a deep skin infection causing severe pain and skin darkening
- Stevens-Johnson syndrome (SJS) – a rare, serious drug reaction with blisters and skin peeling
- Toxic epidermal necrolysis (TEN) – a severe form of SJS affecting large skin areas
- DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms)syndrome – a delayed drug reaction with rash, fever, swelling, and internal organ involvement
- Lyme disease with systemic symptoms – especially if accompanied by fever or joint pain
- Advanced psoriasis or rosacea – often requires a long-term care plan from a dermatologist
If you’re not sure whether your rash is urgent or not, urgent care can still be a good place to start. The provider can help you decide if you need additional care or testing elsewhere.

What urgent care clinics can do for rashes
Urgent care clinics can diagnose and treat various rashes, including infections, allergies, and dermatitis. They offer exams, basic tests, and prescriptions. While not suitable for severe or complex cases, they’re a good first step for fast relief and to determine if you need specialist care.
Urgent care clinics play a vital role in the initial assessment and management of skin rashes. While they can effectively diagnose and treat many common dermatologic conditions, limitations exist in diagnostic testing capabilities. Patients with complex, persistent, or severe rashes may require referral to dermatology or emergency services for further evaluation and management.
This is what you can expect from an urgent care clinic if you visit with a rash:
Rash diagnosis
Urgent care can help with rashes based on the patient’s history and a physical or virtual examination. Providers use rash appearance, location, and accompanying symptoms to determine the course of treatment and whether you need emergency attention.
Rash testing
Testing at urgent care clinics typically includes basic diagnostic tests, such as blood tests, skin swabs, or patch testing, when providers suspect an infection or allergies. Primary care clinics normally test for rashes that persist or present systemic symptoms.
It’s essential to note that urgent care testing for rashes is generally diagnostically useful for identifying possible bacterial, fungal, or streptococcal infections. However, not all urgent care clinics have access to a range of tests. For example, KOH tests for ringworm are infrequent. Skin cultures for impetigo and MRSA cellulitis have a long turnaround of up to 24 hours. Serologies that test rash presentations for Epstein-Barr and HIV are rare in urgent care settings. In addition, most clinics lack virtual dermatology consultation support.
Also, if a rash appears mild at first but rapidly worsens or involves new symptoms —such as blisters, facial swelling, or confusion — seek emergency care. Some serious conditions (like SJS or DRESS) may start with subtle symptoms.
Rash treatment
Treatment from urgent care prioritizes symptom relief and, whenever possible, addressing the underlying cause. Clinics use a range of medicinal products, including antihistamines, antifungal creams, antibiotics, and corticosteroid injections.
- Topical treatments
Topical treatments form the backbone of rash management. Calamine lotion provides basic comfort for itchy rashes. Antifungal ointments address ringworm. Antibiotic creams fight bacterial skin conditions. For dermatitis-type flares, hydrocortisone cream is a reliable tool.
- Oral medications
Oral treatments are used when rashes are more widespread or don’t respond to topicals alone. Antihistamines help control allergic reactions, oral antibiotics are used to treat skin infections such as impetigo or cellulitis, and corticosteroids may be prescribed to reduce severe inflammation.
If symptoms don’t improve within a few days or if the diagnosis remains unclear, follow-up with a primary care provider or dermatologist is recommended. Also, note that some urgent care clinics may not accept children under the age of 2, so families should check before visiting with very young patients.
When can you treat a skin rash at home?
Most mild, localized rashes, like contact dermatitis, eczema, or fungal infections, can be treated at home. Just be sure there’s no fever, pain, blistering, mucosal involvement, or spreading.
Here are common situations where you can treat a rash at home:
- The rash is mild and not spreading quickly
- There is no fever, pain, or swelling accompanying the rash
- You’ve had a similar rash before and know what caused it
- The rash is limited to one small area
- There are no open sores, blisters, or signs of infection, such as pus or increasing redness
- You feel well otherwise
At-home treatments to calm a skin rash
Try using moisturizers, over-the-counter hydrocortisone, antihistamines, and barrier creams to help calm many mild skin rashes at home. These are generally safe when there’s no pain, fever, or rapid spread. Severe, painful, or blistering rashes require medical care.
Here are a few at-home treatments for rashes, recommended by Dr. Knox:
- Cool compresses to relieve itching and reduce inflammation
- Fragrance-free moisturizers or colloidal oatmeal baths for dry, itchy skin
- Hydrocortisone 1% cream for inflammation or irritation (but avoid using on the face or genitals, unless directed by a doctor)
- Antihistamines, like diphenhydramine or loratadine, for itching, especially with hives
- Avoiding triggers, such as new skin products, synthetic fabrics, or known allergens
To learn about identifying and treating allergies, see our article Allergies: Symptoms and Types.
How Doctor On Demand can assist with your rash right now
If you have a new rash or one that’s getting worse, Doctor On Demand offers fast, medically sound care without the wait. Most common rashes and skin care conditions treated in urgent care can be diagnosed and managed effectively through virtual visits, no matter where you are, when you provide clear photos and a detailed history.
During your virtual appointment, your board-certified physician or dermatologist will examine your rash via secure video, review photo uploads, and prescribe medications such as topical steroids, antifungals, or oral antihistamines for allergy treatment.
If your rash shows signs of something more serious, such as spreading bruises, blisters around the eyes or mouth, or signs of infection, Doctor On Demand can help triage your condition and guide you to urgent or emergency care, based on recommendations from the American Academy of Dermatology.
Whether your rash needs simple treatment or rapid escalation, Doctor On Demand helps you take the right next step, right away, without leaving home.
How to prepare for your Doctor On Demand visit for a rash
Preparation will set you up for an effective and successful virtual consultation. Make notes about the symptoms and timeline of the rash, and ensure your phone or computer is ready to conduct a call with a provider.
Follow these preparation guidelines to get the most from your call:
- High-quality images: Take clear, well-lit photographs of the rash from multiple angles. Consider including a ruler or coin for scale. If you take close-up images, get both the affected area and the context of healthy skin.
- Symptom documentation: List when the rash started, how long you’ve had it, and any additional symptoms, such as itchiness or fever. Also, consider any potential triggers or exposures.
- Medical history: Have a list handy of your current medications, allergies, previous skin conditions, and your general medical history.
- Environmental factors: Document any recent changes in skin care products, detergents, or environmental exposures that might be relevant.
- Technical readiness: Ensure that your device’s camera and microphone function correctly, and that you have a stable internet connection for the video consultation.
Doctor-answered skin rash FAQs
Here are frequently asked questions on skin rash, answered by doctors.
- Can a rash be dangerous, or are they usually harmless?
Most rashes are harmless, but may be dangerous if they appear with fever, mucosal lesions, peeling skin, or significant blistering. Seek immediate emergency care for some life-threatening rashes, including:
• Toxic epidermal necrolysis (TEN)
• Stevens-Johnson syndrome (SJS)
• Meningococcemia (meningococcal septicemia or blood poisoning)
• Vasculitis (inflammation of the blood vessels)
- How can I tell if my rash is caused by an allergy, infection, or something else?
Allergic, infectious, and other rashes can all appear similar, characterized by redness, itching, and swelling. Allergic rashes, like hives, are often itchy and symmetrical. Infectious rashes, like ringworm and impetigo, may be scaly and one-sided. Autoimmune rashes, such as lupus, can affect the face and joints and often present with fatigue.
You should consult a medical professional to accurately classify your rash and determine the most suitable treatment, taking into account testing results, exposure history, and clinical judgment.
- Should I try over-the-counter (OTC) creams before seeing a doctor?
You should try OTC creams for mild rashes, but consider seeing a doctor if the rash does not improve after 3-5 days. Suitable non-prescription remedies include hydrocortisone 1% cream, antifungal creams, and oral antihistamines. However, if the itching and irritation worsen or spread rapidly, see a doctor.
- Can stress really cause a rash?
Yes, most researchers agree that stress can cause rashes and worsen existing skin diseases. Increases in cortisol can provoke stress-induced conditions such as atopic dermatitis, psoriasis, and idiopathic urticaria, also known as chronic hives.
- Can I transmit a rash to other people?
Although allergic and autoimmune rashes are not contagious, some rashes are infectious. Take extra care if you have scabies, impetigo, or viral rashes, such as hand, foot, and mouth disease. You must not share towels, clothes, or engage in skin contact before receiving a medical diagnosis.
- Do I always need a prescription to treat a rash?
Many mild rashes, such as contact dermatitis or insect bites, respond well to over-the-counter treatments like hydrocortisone, antihistamines, and moisturizers. However, you may need prescription medication, such as an antifungal or prednisone, if the rash is widespread, painful, or not improving.
About the authors

Dr. Brian Knox is board-certified in Internal Medicine and Pediatrics, and has been overseeing clinical services at Included Health for the past 3 years. Prior to joining IH 6 years ago, Dr. Knox spent 9+ years providing primary care to adults and children. He has expertise in preventive care, primary care for the LGBTQ+ population, as well as the management of patients with difficult-to-control diabetes and hypertension.

Dr. Jeanette Carpenter is board certified in Family Medicine and practices in Virginia. She has an interest in preventative medicine and holistic medicine and has a certification in plant based nutrition from eCornell. She believes stress and lifestyle impacts the disease process and spends extra time educating patients on lifestyle modifications that can improve their overall health.

Quan Lam is a copywriter with over 15 years of experience writing and editing content for both start-ups and legacy brands, as well as 2 years of writing experience exclusively within the healthcare space. She currently lives and works in New York City.



