Chest congestion can be a minor problem or a sign of a more serious health issue. When dealing with chest congestion, it’s important to understand potential warning signs, as well as what type of medical care to seek for them. There are times when caring for chest congestion can be done at home without needing to see a doctor.
When to see a doctor for chest congestion
If you’re experiencing shortness of breath, a fever of 100.4°F or higher, chest pain, or blood in your saliva, you should consider seeking medical attention for chest congestion. For those with underlying conditions, like chronic bronchitis and emphysema, or who have worsening symptoms, it’s recommended that you see a doctor promptly.
Difficulty breathing that worsens rapidly or doesn’t go away with rest is another warning sign. This may mean you’re not getting enough oxygen, which can cause serious complications. Receiving treatment quickly can make a life-saving difference. If someone gasps for air, struggles to speak in complete sentences, or uses their chest and neck muscles to breathe, they need emergency care. When inhaling, wheezing or a high-pitched sound (stridor) may indicate a blocked airway. If you notice that your lips or fingers look blue or gray (a condition called cyanosis), you need emergency care.
You should never ignore chest pain or chest soreness with congestion. If the pain feels tight, crushing, or extends to the jaw, arm, or back, it could be a heart attack. This concern is especially serious for people with high blood pressure, diabetes, or who have a history of heart disease. Seek care right away if you’re coughing up bloody mucus or have heart or lung conditions like asthma or chronic obstructive pulmonary disease (COPD). People with chronic respiratory conditions or weakened immune systems should seek care sooner, as congestion can quickly worsen.
When to use telehealth for chest congestion
Use telehealth, also known as virtual care, for chest congestion when symptoms are mild to moderate and you need medical advice, prescriptions, or a treatment plan. Virtual visits can diagnose colds, flu, or allergies and help you manage symptoms at home. For more severe symptoms, in-person care may be the recommended course of treatment, and your virtual provider can help you make that decision.
With telehealth, you can quickly get an initial evaluation, prescriptions, or follow-up care. Virtual care is a convenient, affordable option for dealing with congestion caused by colds, flu, allergies, or mild respiratory infections. An online doctor can assess symptoms, suggest over-the-counter treatments, and prescribe antibiotics, if needed, for bacterial infections.
If your symptoms indicate more serious problems, the telehealth provider may refer you for in-person care or testing. Also, people with asthma, COPD, or other lung conditions can use telehealth for a virtual check-up when symptoms flare.
How to prepare for your doctor’s visit for chest congestion
Before your doctor’s visit for chest congestion, list your symptoms and when they started, note all medications (OTC, prescriptions, or supplements), and write down your questions for the doctor. If you have asthma, COPD, or allergies, be sure to mention recent flare-ups. This preparation helps the doctor treat you.
If you’re using telehealth, find a quiet spot with good lighting where you can speak freely with a doctor. If you happen to have a thermometer, pulse oximeter, and a list of recent temperatures or oxygen readings available, share those with your provider.
Questions for your appointment
Write down questions for your doctor and check them off during your appointment. You should consider asking about the likely cause, tests, and medications to take.
Here are specific questions to ask the doctor about chest congestion:
- What is causing my chest congestion? This answer will help guide your treatment. For example, you might have a virus, a bacterial infection, or allergies. Less common causes include Respiratory Syncytial Virus (RSV) or an underlying condition.
- Do I need any tests, such as a chest X-ray or lab work? If your congestion is severe or lasts longer than expected, your doctor may recommend tests to check for pneumonia or other lung conditions. Ask what to expect with the tests and when you’ll get your results.
- Should I take antibiotics? Many cases of chest congestion are viral and don’t respond to antibiotics. However, medication can help if a bacterial infection like pneumonia is suspected.
- How can I treat my symptoms at home? Ask about over-the-counter medications and simple home care like steam therapy.
- What warning signs should I watch for? Ask the doctor what symptoms should trigger a follow-up appointment.
- Am I at risk for complications due to my medical history? If you have asthma, COPD, heart disease, or a weakened immune system, your doctor can discuss precautions.
- Can I continue my daily activities, or should I rest? Depending on the severity of your symptoms, your doctor may recommend rest, work modifications, or specific recovery guidelines.
- Is telehealth a good option for follow-up care? Virtual visits offer an easy way to check in with your doctor if your symptoms aren’t severe but require monitoring.
What causes chest congestion?
Chest congestion happens when mucus builds up in your respiratory system. Common causes are colds, flu, or allergies.
Mucus is the body’s way of trapping germs and irritants, but too much can lead to chest congestion, wheezing, shortness of breath, or persistent coughing with or without mucus. The American Thoracic Society’s 2015 study, “The Relationship of Mucus Concentration (Hydration) to Mucus Osmotic Pressure and Transport in Chronic Bronchitis,” found that clearing excess mucus is a significant factor in protecting the lungs from “inhaled infectious and noninfectious challenges.”
The following are possible causes of chest congestion:
- Viral infections: Colds, the flu, sinus infections and COVID-19 often cause chest congestion by inflaming the airways, increasing mucus production, and aggravating flu-like symptoms like mild headaches, body aches, chills, and vomiting. Most cases can improve with medication, rest, liquids, and over-the-counter remedies.
- Bacterial infections: Severe congestion can come from bacterial bronchitis or pneumonia. They typically require antibiotics and further medical evaluation.
- Allergies and asthma: Pollen, dust, and other allergens can inflame your airways, which leads to congestion, sore throat, wheezing, and difficulty breathing. Asthma can also cause excess mucus and tightness in the chest.
- Chronic respiratory conditions: COPD, chronic bronchitis, and emphysema can lead to persistent chest congestion. They often require long-term medical care.
- Environmental exposure: Cigarette smoke, air pollution, chemicals, or other irritants can cause mucus buildup and lung inflammation, especially for people with asthma or chronic respiratory conditions.
- Gastroesophageal Reflux Disease (GERD): Acid reflux can lead to a chronic cough and chest congestion, especially at night.
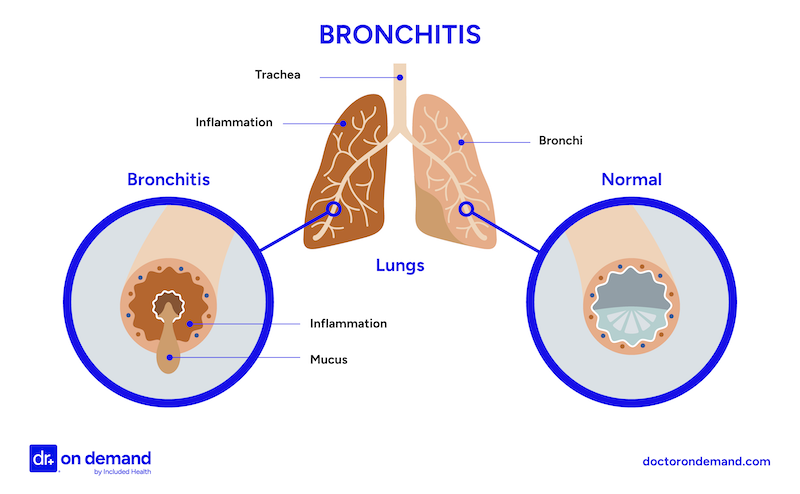
What Chest Congestion Looks Like
How to get rid of chest congestion
There are some treatment options that you can do right at home to help clear chest congestion, including drinking plenty of fluids and using steam or humidifiers. You should also consider over-the-counter decongestants or cough medicines, which don’t require a prescription. Get medical help immediately if you have trouble breathing, a high fever, chest pain, or if symptoms get worse or fail to improve.
At-home treatments recommended by doctors
According to Dr. Ashley Kelley from Included Health, “Hydration is very important, and drinking plenty of water helps to thin mucus and makes it easier to clear the airways. Warm liquids can be especially soothing to irritated airways. For those who desire medication for symptom relief, I suggest my patients try a common OTC medicine called guaifenesin, which can help to further thin the mucus.”
“Hydration is very important, and drinking plenty of water helps to thin mucus and makes it easier to clear the airways.”
While herbal remedies are a common treatment for those looking for at-home solutions, many doctors are cautious about herbal remedies for chest congestion. A 2020 study, “Herbal Medicine for Acute Bronchitis: A Qualitative Interview Study of Patients’ and Health Professionals’ Views,” published in Complementary Therapies in Medicine showed that many UK patients expressed an interest in herbal remedies to avoid unnecessary antibiotics. However, doctors interviewed in the study had concerns about limited regulation, potential interactions with conventional medications, and insufficient clinical guidance for these therapies. Despite those concerns, the authors of the study concluded, “Many patients and health professionals would consider using herbal medicine for acute bronchitis, if based on trustworthy advice and evidence-based guidelines, respectively.”
What medications may be prescribed for chest congestion?
If chest congestion is severe, prolonged, or caused by an infection, doctors may prescribe medicine to speed up recovery and avoid complications.
“Talking with your health care provider, especially if you have symptoms that are not improving with at-home care, ensures you get on the right track to feeling better.”
“Specific treatment may depend on the underlying cause of the chest congestion,” says Dr. Ashley Kelley, “so it is important to discuss your specific needs with your healthcare provider. Patients with asthma may need to increase the frequency of their inhaler use or take a short course of oral steroids. Patients who have specific viral infections, such as influenza or COVID-19, may benefit from early anti-viral treatment, and patients with bacterial infections in their sinuses or chest may need antibiotics. Talking with your health care provider, especially if you have symptoms that are not improving with at-home care, ensures you get on the right track to feeling better.”
How Doctor On Demand can help with chest congestion right now
If you’re experiencing chest congestion and need answers immediately, start a virtual visit with a board-certified healthcare provider today with Doctor On Demand. Whether your symptoms are mild or worsening, our 24/7/365 virtual care can provide fast answers and treatment options conveniently from home.
If medication is necessary, Doctor On Demand providers can also write prescriptions for antibiotics, inhalers, or steroids and send them directly to your preferred pharmacy. They can discuss OTC treatments to ease congestion. During your visit, the provider will:
- Evaluate your symptoms: Discuss how long your chest congestion has lasted and if you have a fever, wheezing, or difficulty breathing.
- Determine the likely cause: The doctor will diagnose whether it’s likely a viral infection, bacterial illness, allergies, or another condition.
- Recommend treatment: Get guidance on at-home care, prescriptions if needed, and when to seek further care.
While many cases of chest congestion can be treated with a virtual visit, your doctor will let you know if additional care is needed. If you have a severe infection or a worsening condition, the doctor will advise you on what to do next.
Interested in connecting with a board-certified healthcare provider in minutes through Doctor On Demand? Sign up today.
How to prepare for your Doctor On Demand visit
A virtual visit with Doctor On Demand is quick and convenient. Following the steps below can make it even easier for you to get the care you’re looking for.
- Find a good spot in your home: Choose a quiet, well-lit spot so your doctor can see and hear you.
- Document your symptoms: Before your visit, jot down a few details about your chest congestion, including:
- When did your symptoms start, and have they worsened over time?
- Note details about fever, shortness of breath, feeling tired (fatigue), wheezing, or coughing up mucus.
- Tell the doctor if you’ve had other recent illnesses or allergies.
- Have a thermometer handy: If possible, have a thermometer and a pulse oximeter. These can help your doctor evaluate the severity of your symptoms. The doctor may request that you perform simple self-examinations under their guidance, so additional lighting from a lamp, flashlight, or smartphone may be useful.
- List medications and history: Share any prescription or over-the-counter medications you’re taking. Also, be ready to discuss any existing conditions you have.
- Prepare questions for your doctor: List any questions you have about your chest congestion and treatment plan. You can also review our questions to ask about your chest congestion section above.
See a doctor now for your chest congestion
Board certified online doctors and clinicians are available 24/7.
Get startedDoctor-answered chest congestion FAQs
Here are frequently asked questions regarding chest congestion.
- How long does a chest cold normally last?
Most chest colds clear up in 7-10 days, though a cough can linger for a few weeks. If your symptoms don’t improve or worsen after the first week, it’s time to see a doctor. - Can chest congestion be a sign of something serious?
Sometimes, yes. Pneumonia, acute bronchitis, heart failure, lung cancer, or COVID-19 are all examples of more serious ailments that can cause chest congestion.If you have a high fever, bloody mucus, or severe breathing difficulty, seek care immediately. - Can chest congestion be a sign of something serious?
Sometimes, yes. Pneumonia, acute bronchitis, heart failure, lung cancer, or COVID-19 are all examples of more serious ailments that can cause chest congestion. If you have a high fever, bloody mucus, or severe breathing difficulty, seek care immediately. - How do you know when chest congestion turns into pneumonia?
Watch for fever above 100.4°F, worsening shortness of breath, sharp chest pain, rust-colored mucus, and extreme fatigue. Seek medical care as soon as possible if you develop these symptoms. - Does green phlegm indicate an infection?
The color of your saliva or mucus alone doesn’t confirm an infection. Both viral and bacterial illnesses—and even allergies—can cause green or yellow mucus. See a doctor if you have persistent fever, trouble breathing, or worsening symptoms. Only a full evaluation can determine if an antibiotic is necessary. - How do I know if I need antibiotics for chest congestion?
Antibiotics work only for bacterial infections. Persistent fever above 101°F and worsening symptoms can indicate an underlying bacterial cause. Your doctor can confirm whether antibiotics are right for you. - Could my chest congestion be a sign of COVID-19?
COVID-19 often has symptoms that include congestion, fever, dry cough, fatigue, or loss of taste or smell. If you’ve been exposed or have these symptoms, get tested and isolate until you’re sure it’s safe to be around others. - Can a sinus infection cause chest congestion?
Yes. A postnasal drip from a sinus infection can allow infected mucus to move from your sinuses into your lungs. Addressing sinus problems early reduces the risk of more serious respiratory issues. - How is chest congestion different from an upper respiratory infection?
An upper respiratory infection usually affects your nose, sinuses, or throat, causing nasal congestion, a runny nose, or a sore throat. Chest congestion involves the lower airways and feels heavier, with a deeper cough and potential wheezing. - Is chest congestion contagious?
Chest congestion itself is a symptom, not a contagious disease. However, if an underlying infection (viral or bacterial) is causing the congestion, that infection can spread through droplets when coughing or sneezing. - What tests are done for severe chest congestion?
Your doctor may order a chest X-ray, CT scan, or sputum culture. In some cases, pulmonary function tests or bronchoscopy can be helpful. These help reveal the cause of congestion and guide the most effective treatment. - How do doctors determine the cause of chest congestion?
Doctors typically start with your medical history. Then, they’ll perform a physical examination, monitor your breathing and oxygen saturation, and listen to your lungs. Lab tests or X-rays may confirm infection or inflammation. - Can chest congestion cause RSV?
Chest congestion doesn’t cause Respiratory Syncytial Virus (RSV). Instead, RSV may cause congestion, especially in infants, older adults, and those with weakened immunity. If you suspect RSV, see a doctor promptly.
See a doctor now for your chest congestion
Board certified online doctors and clinicians are available 24/7.
Same-day prescriptions availableAbout the authors

Adrian Black-Seitz has worked as a copywriter and blogger for over three years in the healthcare industry. He lives and works in Virginia and is passionate about the work Included Health is doing.

Dr. Heather Hockenberry is board certified in family medicine. She earned her doctor of medicine degree at the University of Nevada Reno School of Medicine where she also completed her internship and residency in family medicine, serving as chief resident during her time there. As an urgent care physician for a decade prior to coming to Included Health, she treated acute illnesses and injuries of a diverse nature in a clinic setting. She came to Included Health in 2015 as a staff physician, and currently serves as an associate medical director supporting our clients from a clinical perspective.



