Table of contentIn this article
- When should I see a doctor for a yeast infection?
- What are the signs of a yeast infection
- Conditions often confused with yeast infections
- How do doctors treat yeast infections?
- Treatments for high-risk groups for a yeast infection
- Possible complications from untreated yeast infections
- Treating your simple yeast infection at home
- How Doctor On Demand can assist with your yeast infection
- Doctor-Answered Yeast Infection FAQs
Not sure if your yeast infection requires a doctor’s visit? This guide explains when to seek care, what symptoms to watch for, how treatment works, and which infections can be confused with a yeast infection. It includes tips for urgent care, telehealth, and more.
When should I see a doctor for a yeast infection?
Reach out to a doctor if this is your first time dealing with yeast infection symptoms, if the discomfort is unusually strong, or if things haven’t eased up after several days of home treatment. You’ll also want medical input if you’re expecting a baby, have recurring infections, or manage a health condition that weakens your immune defenses.
Most vaginal yeast infections (also called vaginal candidiasis) respond well to simple treatments, but not all cases are alike. When symptoms don’t follow the usual pattern, seem to worsen, or don’t clear with standard remedies, a medical exam can help pinpoint what’s going on. If you’re pregnant or have underlying health concerns, like high blood sugar or a suppressed immune system, it’s safest to check in before starting any treatment.
The fungus most often responsible, Candida albicans, is part of the body’s natural mix of organisms. It’s found on the skin and in areas like the mouth, digestive system, and genital tract. Normally, it stays in check, but when something shifts that balance, yeast can multiply and trigger infection.
Although vaginal infections are the most well-known, yeast can also cause issues in other groups. Men may develop irritation or rashes on the penis. Infants, older adults who wear diapers, and people with long-term illnesses are also more likely to develop yeast-related skin problems. In any of these cases, a medical provider can help confirm the diagnosis and suggest the right care.
When to go to urgent care for a yeast infection
It’s a good idea to visit urgent care if you’re dealing with intense vaginal symptoms, like swelling, redness, or burning that feels hard to manage. A sudden fever or ongoing discomfort can also be a sign that something more serious is going on, especially if you have a medical condition that affects healing.
While yeast infections aren’t life-threatening, the discomfort can be significant. If symptoms become hard to tolerate or appear suddenly, urgent care offers a fast way to get evaluated and start treatment. It’s also a helpful option when you can’t get in to see your primary doctor or if things don’t improve after you’ve tried treatment on your own.
When you can use telehealth for a yeast infection
Telehealth can be a convenient way to diagnose and treat mild-to-moderate yeast infections. This is especially true for patients who have experienced yeast infections before and are familiar with the symptoms, and who do not have complicating health factors such as pregnancy, diabetes, or weakened immune systems.
If you’ve dealt with a yeast infection before and the symptoms feel familiar, telehealth can be a fast, practical option. A clinician can talk through your symptoms and, if it seems consistent with past infections, send treatment to your pharmacy the same day. But if this is your first time or something feels unusual, it’s safer to be examined in person to rule out other causes.
When to go to a gynecologist for a yeast infection
You should see a gynecologist if you’re experiencing vaginal yeast infection symptoms for the first time, if your symptoms are unusually intense, or if you’re pregnant or managing a chronic health condition.
Gynecologists are trained to evaluate vaginal symptoms and can tell whether you’re dealing with a yeast infection or something else, such as a bacterial imbalance or an STI. If this is your first time having symptoms, or they feel different from past infections, a pelvic exam and lab tests can help ensure you get the right diagnosis and treatment.
If you’re expecting, have high blood sugar, or take medications that affect your immune system, it’s even more important to get expert advice. Certain treatments, including some oral medications, aren’t recommended during pregnancy. A gynecologist can guide you toward safe and effective options based on your specific needs.
What are the signs of a yeast infection
Yeast infections in the vagina often lead to itching, irritation, and a discharge that’s thick, pale, and lumpy. Other signs may include discomfort during urination or sex, swelling near the vaginal opening, and soreness that gets worse if left untreated.
Common symptoms include:
- Itching in or around the vagina: Often the first sign, and it can be persistent or hard to ignore.
- Burning while urinating: A sharp or stinging sensation may occur, especially on irritated skin.
- Inflammation or puffiness: The affected area may look red, feel tender, or appear swollen.
- Soreness or sensitivity: Daily activities or movement may feel uncomfortable in the vaginal area.
- Thick discharge: Often described as white and clumpy, with little or no odor.
- Discomfort during sex: Irritation or lack of moisture can make intercourse painful.
Symptoms of a serious yeast infection
A serious yeast infection may cause severe swelling, raw or broken skin, intense pain, or a fever. These symptoms often signal a more complicated infection or a different condition entirely. Prompt medical care can help confirm the cause and prevent symptoms from getting worse.
Signs of a severe or complicated yeast infection include:
- Significant swelling and redness: The vulva may look inflamed, feel hot to the touch, and become increasingly uncomfortable.
- Cracked or broken skin: The affected area may split open or become raw from irritation or scratching.
- Severe pain or burning: Discomfort may interfere with walking, sitting, or daily activities.
It’s important to note that a fever isn’t typical of a yeast infection and may point to another condition, such as a bacterial infection or pelvic inflammatory disease.
What do frequent yeast infections signal?
If you get four or more yeast infections in a year, you may have a recurring or complicated condition. Frequent infections can be linked to diabetes, immune system problems, hormonal changes, or a less common strain of yeast that doesn’t respond well to standard treatment.
Recurring yeast infections often have an underlying cause. Your doctor may run tests to check for chronic conditions or take a culture to identify which strain of yeast is present. Some people may need long-term or alternate treatments if their infections keep coming back. Getting evaluated can help you break the cycle and avoid unnecessary discomfort.
Some common potential underlying causes include:
- Diabetes: High blood sugar can fuel yeast overgrowth and make infections harder to treat.
- Weakened immune system: If your body can’t fight off infections effectively, yeast can grow unchecked.
- Hormonal factors: Oral contraceptives, hormone therapy, or even menstrual changes may play a role.
- Tight or non-breathable clothing. Trapped moisture in the genital area may promote yeast growth.
- Frequent antibiotic use: Antibiotics can disrupt natural bacteria that normally keep yeast in balance.
- Genetic susceptibility: Some people are simply more prone to yeast infections due to inherited factors.
Symptoms that are not typical of a yeast infection
Symptoms that aren’t typical of a vaginal yeast infection include a fishy odor and a yellow-green or frothy discharge and may indicate a different condition or infection. Also watch for blisters or sores, fever, chills, pelvic pain, irregular bleeding, and painful urination. See a doctor for these symptoms.
These symptoms aren’t usually caused by a yeast infection and may point to something else, such as a bacterial infection, STI, or pelvic inflammatory disease. Getting checked can help you avoid the wrong treatment and catch a more serious issue early.
What to watch for:
- Strong odor: A fishy or foul smell is more typical of bacterial vaginosis than a yeast infection.
- Unusual discharge: Trichomoniasis often causes yellow-green or bubbly discharge that doesn’t match the thick, white discharge seen in yeast infections.
- Blisters or sores: Painful lesions around the genitals may signal herpes or another viral infection.
- Fever and chills: These are uncommon with yeast infections and may indicate a more widespread infection.
- Lower abdominal pain: This can point to pelvic inflammatory disease or another condition requiring antibiotics.
- Spotting or bleeding: Unexplained bleeding may be linked to hormonal changes or a sexually transmitted infection.
- Sharp burning while urinating: This symptom is more consistent with a urinary tract infection than with yeast.
Conditions often confused with yeast infections
You may mistake several conditions for vaginal yeast infections because they have similar symptoms. These conditions include bacterial vaginosis, trichomoniasis, urinary tract infections, sexually transmitted infections, allergic reactions, and atrophic vaginitis.
According to Dr. Melissa Eirich, “I’ve seen many patients who were treated for a yeast infection over and over, only to find out it was actually something else, like a bacterial infection (BV) or even an allergic reaction. Some patients have even discovered they had a latex allergy from condoms, mistaking it for just another yeast infection. That’s why it’s incredibly important to get a full gynecological exam if your symptoms keep coming back.”
Here’s a breakdown of conditions often mistaken as yeast infections:
- Sexually transmitted infections (STIs)
- Trichomoniasis: Similar to a yeast infection, trichomoniasis may cause vaginal irritation, itching, and discharge. However, unlike a yeast infection, it is often accompanied by a frothy, yellow-green discharge with a strong odor.
- Chlamydia: Some symptoms may overlap between chlamydia and a yeast infection, but chlamydia more often causes a watery or mucus-like discharge with a mild odor, a painful burning sensation when urinating, and bleeding between periods.
- Gonorrhea: Symptoms include a yellowish-green, watery vaginal discharge, painful urination, pelvic pain or discomfort, and bleeding between menstrual periods or after intercourse.
- Genital herpes: Genital herpes causes painful blisters or sores in the genital or anal regions. It can also cause flu-like symptoms.
- Vaginal bacteria issues
- Bacterial vaginosis: BV is often mistaken for a yeast infection, as both conditions cause itching, irritation, and discharge. BV symptoms include thin, watery, grayish-white vaginal discharge; a strong, fishy odor, especially noticeable after intercourse; and mild irritation or burning that is usually less intense than a yeast infection. The condition is caused by an imbalance of natural bacteria in the vagina.
- Cytolytic vaginosis: Cytolytic vaginosis is often misdiagnosed as a recurring yeast infection, as the two conditions share similar symptoms. Symptoms of cytolytic vaginosis include vaginal itching, burning, and irritation. It causes a thick, white discharge that may resemble a yeast infection, but tends to be less lumpy.
- Skin conditions
- Eczema: Eczema can be mistaken for a yeast infection as both conditions cause red, itchy, irritated skin. Eczema can occur anywhere on the body and often presents as dry, scaly, thickened patches. Unlike a yeast infection, eczema does not cause discharge, unless the skin has a secondary infection.
- Psoriasis: A yeast infection and psoriasis in the genital area can both cause itching and redness. Psoriasis is an autoimmune skin disorder known for raised, red patches with silvery-white scales or smooth, red lesions without scales. Unlike a yeast infection, it does not cause discharge, unless the skin has a secondary infection.
- Contact dermatitis: Contact dermatitis from scented pads, soaps, or clothing dyes in the genital area can have the same symptoms as a yeast infection and may mimic or coexist with a yeast infection. Contact dermatitis is an inflammatory skin reaction caused by contact with an irritant or allergen, whereas a yeast infection is a fungal overgrowth. Unlike a yeast infection, contact dermatitis does not cause discharge, unless the skin has a secondary infection.
- Lichen sclerosus: Similar to a yeast infection, lichen sclerosus can affect the genital area, especially in women, and cause itching, redness, and discomfort. An autoimmune disorder, lichen sclerosus causes white, thin, wrinkled-looking skin. Unlike a yeast infection, it does not normally cause discharge.
Several conditions can mimic the symptoms of a yeast infection, including itching, irritation, and discharge, but they differ in cause, treatment, and other key signs. This table compares common differences to help highlight when it may be something else.
| Condition | Type of Discharge | Odor Present? | Other Key Symptoms | How It Differs from a Yeast Infection |
| Bacterial vaginosis | Thin, gray or off-white | Yes—fishy, especially after sex | Mild irritation or burning | Caused by bacterial imbalance; needs antibiotics |
| Trichomoniasis | Frothy, yellow-green | Often strong and unpleasant | Itching, soreness, spotting | Caused by a parasite; is sexually transmitted |
| Chlamydia | Mucus-like or watery | Usually mild or none | Bleeding between periods, painful urination | Often silent; diagnosed through lab testing |
| Gonorrhea | Yellow or green, possibly watery | May be mild | Pelvic pressure, abnormal bleeding, urinary pain | Bacterial STI; often overlaps with chlamydia |
| Genital herpes | None or light, watery | No | Painful sores or blisters, flu-like symptoms | Viral; symptoms include visible lesions not seen in yeast cases |
| Cytolytic vaginosis | White, thick but smooth | No | Irritation, low vaginal pH | Caused by overgrowth of healthy bacteria |
| Eczema (genital) | None | No | Itchy, dry, or cracked skin | Skin reaction, not infection; may be triggered by irritants |
| Psoriasis | None | No | Red patches or plaques, sometimes with silvery scale | Autoimmune; can resemble yeast but doesn’t cause discharge |
| Contact dermatitis | None | No | Burning, redness, itching after exposure | Caused by irritation or allergy, not infection |
| Lichen sclerosus | None | No | Wrinkled, thin, pale skin; itching or pain | Autoimmune; requires long-term care and often affects vulvar skin |
| Urinary tract infection | None (or cloudy urine) | Possible urine odor | Painful urination, urgency, abdominal cramping | Involves urinary tract, not vaginal tissue |
How do doctors treat yeast infections?
Doctors treat yeast infections by prescribing or recommending antifungal medication. Depending on the case, they may suggest a pill taken by mouth or a treatment used inside the vagina. Some options are over the counter; others require a prescription. The right option depends on how severe the infection is and whether it’s a first-time or recurring issue.
For a straightforward case, a short course of treatment is often enough. Your doctor may suggest a single-dose oral antifungal, a vaginal suppository, or a multi-day cream. If symptoms don’t improve or the infection keeps coming back, they may recommend a longer regimen or test to confirm the type of yeast involved.
Doctor’s treatments for mild or occasional yeast infections
Doctors usually treat a mild or occasional yeast infection with an antifungal cream, a single-dose medication taken by mouth, or a suppository (small object put into the vagina to deliver medicine). You can expect 3–7 days for the infection to go away.
Over-the-counter treatments are often effective for uncomplicated cases. These include clotrimazole or miconazole creams and suppositories, sold under brand names like Monistat. Many people start to feel better within a day or two, but it’s still important to finish the full course if the treatment calls for multiple doses. Your doctor can also help you choose between oral and vaginal options based on your symptoms, preferences, and medical history.
Doctor’s treatments for complicated or recurrent yeast infections
Doctors treat complicated or recurrent yeast infections with longer or combined therapies. These may include oral antifungal medication, extended vaginal treatments, or boric acid suppositories. Pregnant patients require different options, and doctors often look for underlying causes such as diabetes or immune system issues.
In cases that don’t respond to short-term treatment or keep coming back, doctors may recommend a more customized plan. One common approach is a multi-dose regimen of fluconazole, a prescription antifungal taken by mouth over several days. Other options might include a 7–14 day course of vaginal creams or boric acid capsules used internally. Boric acid and oral treatments aren’t typically used during pregnancy, so safer alternatives may be needed.
A 2023 review titled “Treatment of Vulvovaginal Candidiasis—An Overview of Guidelines and the Latest Treatment Methods” in the Journal of Clinical Medicine outlines current treatment guidelines for vaginal yeast infections and highlights newer therapies for difficult cases. In addition to standard antifungals like fluconazole and clotrimazole, the review discusses emerging options such as oteseconazole and ibrexafungerp, which may offer relief for patients with recurrent infections or resistance to first-line treatments.
These findings are consistent with These findings align with a 2022 expert review in Clinical Infectious Diseases, which supports updated CDC guidelines and highlights the importance of boric acid, next-generation antifungals, and molecular diagnostics in treating more complex cases of vulvovaginal candidiasis (VVC), the clinical term for vaginal yeast infections.
When yeast infections recur frequently (four or more times a year), your doctor may check for chronic health problems, such as blood sugar issues or hormonal imbalances. They may also test to confirm whether the infection is caused by a less common yeast species. For some patients, maintenance therapy is recommended to keep symptoms from returning.
Treatments for high-risk groups for a yeast infection
Some people face a higher risk of complications from a yeast infection, including those who are pregnant, have diabetes, or have weakened immune systems. Treatment in these groups may need to be adjusted for safety, effectiveness, or long-term prevention.
Here are the details about high-risk groups:
Pregnant women
As Dr. Jeanette Carpenter explains, “Pregnant women are more susceptible to yeast infections due to hormonal changes, particularly rising estrogen levels, which promote the growth of Candida, the fungus responsible for these infections. It’s crucial for pregnant women to consult a medical professional to identify the safest treatment options. I’ve had patients with a history of recurrent yeast infections stock up on oral antifungal medications like Diflucan for home use. However, this medication is not safe during pregnancy; topical treatments are the safest option at all stages of pregnancy. Therefore, it’s always best to consult with a healthcare professional before taking any medication while pregnant.”
Diabetics
People with diabetes—especially if blood sugar levels are not well controlled—are more prone to developing yeast infections. Dr. Melissa Eirich states, “If you’re a diabetic, it’s really important to know that your chances of getting vaginal yeast infections can actually double.” Elevated glucose levels create an environment where Candida can thrive, making infections more frequent and harder to treat.
According to Women’s Health Specialist, Dr. Jeanette Carpenter: “Managing blood sugar is a key part of preventing recurrent yeast infections. In some cases, a standard course of antifungal treatment may not be enough, and a longer or repeated course may be necessary. It’s important for diabetic patients to speak with a healthcare provider to ensure they receive the right treatment plan and to address any underlying glucose management issues that may be contributing to the problem.”
Immunocompromised
“Individuals with weakened immune systems, such as those undergoing chemotherapy, taking immunosuppressive medications, or living with conditions like HIV/AIDS, are at greater risk of more severe or persistent yeast infections,” according to Dr. Jeanette Carpenter. In these cases, infections may spread beyond the usual areas and become systemic, which can be dangerous. Topical treatments may still be effective, but sometimes oral antifungal medications or longer treatment courses are needed. And unlike in healthy individuals, any recurring or worsening symptoms should be evaluated right away. A medical provider can help tailor treatment and monitor for complications in this vulnerable group.
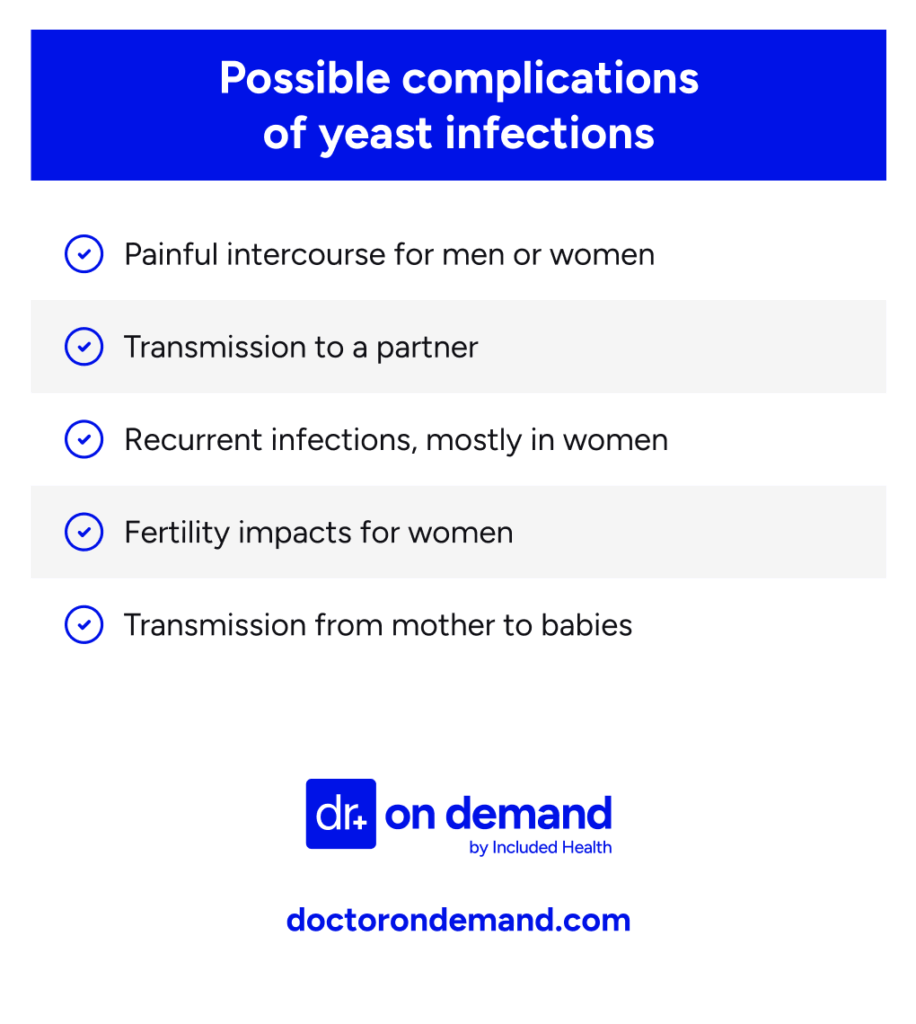
Possible complications from untreated yeast infections
If you don’t treat a yeast infection, you may experience discomfort and end up with more serious complications. This is especially true for pregnant women, diabetics, and people with compromised immune systems.
Complications include:
Painful intercourse: An untreated vaginal yeast infection can cause painful intercourse. This is because the yeast overgrowth causes inflammation and irritation of the tissues in the vagina and vulva. The genitals may be raw and itchy and develop small cuts or cracks. In addition, a yeast infection can interfere with vaginal moisture, leading to a lack of natural lubrication.
Transmission to a partner: A yeast infection is not considered a sexually transmitted infection (STI). Although uncommon, it can be passed to a partner during sex. Both partners should be treated if they have symptoms such as itching, redness, and burning. If one partner does not have symptoms, treatment is usually not necessary.
Recurrent infections: If you don’t treat a yeast infection, you increase your risk of future infections. This is because the longer the infection lasts, the more it can disrupt the normal balance of the vagina or skin. In addition, the ongoing irritation caused by a yeast infection can damage the skin or mucous membranes, making future infections more likely.
Fertility impacts: An untreated vaginal yeast infection usually does not impact fertility in healthy individuals. This is because vaginal yeast infections only affect the outer layers of the vaginal and vulvar tissue and do not impact reproductive organs, such as the uterus, fallopian tubes, or ovaries. However, yeast infections can have an indirect impact on fertility by making sex painful or creating an unfavorable environment in the vagina for sperm. In addition, a more serious condition that impacts fertility, such as a sexually transmitted infection (STI), can be misdiagnosed as a yeast infection.
Transmission to babies: A yeast infection can be transmitted from mother to baby, usually during vaginal birth or through skin-to-skin contact.
Invasive candidiasis: It is rare for a typical yeast infection to cause invasive candidiasis in healthy people. Invasive candidiasis is a life-threatening condition in which Candida (the yeast that causes yeast infections) enters the bloodstream or organs, causing a serious infection that requires hospitalization. A yeast infection may cause invasive candidiasis in people with weakened immune systems or other complicating factors.
Below is an image that illustrates symptoms commonly found with untreated yeast infections.
Treating your simple yeast infection at home
You can treat a mild or uncomplicated yeast infection at home. Home treatment is only appropriate, however, if you are confident that you have a yeast infection, and you do not have severe symptoms.
As Dr. Jeanette Carpenter notes, “There are countless home remedies for yeast infections that I’ve encountered throughout my career in women’s health—everything from boric acid suppositories and tea tree oil to oregano oil, yogurt, coconut oil, and garlic. While they may all work to some extent and are generally considered safe, the goal should be to find something that alleviates symptoms without causing further irritation. I usually recommend avoiding tea tree and oregano oils, as they can be quite concentrated and need significant dilution to be tolerable for vaginal insertion. I’ve had patients who weren’t aware of this and experienced severe irritation as a result. Instead, I suggest using boric acid suppositories designed for insertion or a small amount of yogurt or coconut oil applied on a tampon or with an applicator, as these are considered safe and can be quite effective. If symptoms don’t improve or worsen after a day or two, it’s always best to consult a healthcare professional for a proper examination and treatment.”
How Doctor On Demand can assist with your yeast infection
Our board-certified doctors can provide fast relief from yeast infections, with convenient, same-day prescriptions sent to your local pharmacy. We can help if you are exhibiting symptoms and have questions, have previously had a vaginal yeast infection and are familiar with the symptoms, or if this is your first infection. We offer 24-hour urgent care.
Get treated today by Doctor On Demand for your yeast infection.
How to prepare for your Doctor On Demand visit for a yeast infection
To get ready for your telehealth visit with Doctor On Demand:
- Find a comfortable, quiet space where you can speak freely about your yeast infection symptoms.
- Have your insurance information ready. If you don’t have insurance, you can skip this step.
- A photo ID, like a driver’s license or passport, may also be needed.
- Plan to spend 5-10 minutes answering questions about your symptoms and health history.
Doctor-Answered Yeast Infection FAQs
Here are common questions about yeast infections, answered by our doctors.
Do tight clothes contribute to yeast infections?
Wearing tight or non-breathable clothing, like leggings or synthetic underwear, can trap moisture and warmth. That environment can make it easier for yeast to grow. To lower your risk, choose cotton fabrics and change out of damp clothes as soon as possible.
Can a yeast infection go away on its own?
Sometimes, a mild yeast infection clears up without treatment, especially in people with strong immune systems. But many cases stick around or come back without antifungal medication, so don’t wait too long to act if symptoms continue or get worse.
Can I treat a yeast infection with over-the-counter medication?
Yes, you can manage a mild yeast infection with store-bought antifungal creams or suppositories, but only if you’re sure it’s yeast and you’ve had similar symptoms before. Avoid self-treatment if you’re pregnant or have medical conditions like diabetes.
How long do yeast infections last?
With treatment, symptoms often improve within a day or two and clear up completely in under a week. Without medication, they may drag on or come back. If things haven’t started improving after three days, it’s a good idea to check with a doctor.
How long should I wait to see a doctor for a yeast infection?
If you’ve had a yeast infection before and the symptoms seem familiar, you can try treating it at home and wait a few days to see if it improves. But if it lasts more than a week, comes back soon, or this is your first time, get medical guidance.
How long is too long to leave a yeast infection?
If you’ve been dealing with symptoms for more than a week and things aren’t improving, or they’re getting worse, it’s time to see a doctor. Waiting too long can lead to more discomfort and increase the chance of complications.
Are yeast infections common?
Yes, most women will have a yeast infection at some point. Around three in four will get at least one during their lives, and many will have more than one. They’re especially common during the reproductive years.
Are yeast infections sexually transmitted?
Yeast infections aren’t classified as STIs, but it’s possible to pass yeast between partners through sex. If one person has symptoms, it’s best to avoid sexual contact until treatment is complete. And, both people may need care if symptoms appear.
What if my yeast infection keeps coming back?
Recurring infections, four or more in a year, may signal a deeper issue. Your doctor can check for causes like diabetes, immune problems, or a less common yeast strain that needs a different treatment plan.
What are the stages of a yeast infection?
Early on, you might not notice much beyond mild itching. As the infection progresses, you may develop redness, swelling, thicker discharge, and more irritation, especially during urination or sex. Without treatment, symptoms usually intensify over time.
Can I treat a yeast infection with home remedies?
Some people try natural options like coconut oil or tea tree oil cream, but these aren’t well-studied and may irritate sensitive tissue. If you’re thinking about a home remedy, it’s best to check with a provider first, especially if you’re pregnant or have repeat infections.
Can probiotics help prevent yeast infections?
Probiotics may help maintain a healthy balance of vaginal bacteria, particularly after antibiotics. Some people use supplements or eat foods with live cultures for prevention. They’re not a treatment, but they may help as part of a broader care plan. You can also eat probiotic foods, including yogurt and kombucha.
Also, learn more about supporting your gut health.
About the authors

Dr. Heather Hockenberry is board certified in family medicine. She earned her doctor of medicine degree at the University of Nevada Reno School of Medicine where she also completed her internship and residency in family medicine, serving as chief resident during her time there. As an urgent care physician for a decade prior to coming to Included Health, she treated acute illnesses and injuries of a diverse nature in a clinic setting. She came to Included Health in 2015 as a staff physician, and currently serves as an associate medical director supporting our clients from a clinical perspective.

Dr. Brian Knox is board-certified in Internal Medicine and Pediatrics, and has been overseeing clinical services at Included Health for the past 3 years. Prior to joining IH 6 years ago, Dr. Knox spent 9+ years providing primary care to adults and children. He has expertise in preventive care, primary care for the LGBTQ+ population, as well as the management of patients with difficult-to-control diabetes and hypertension.


