Table of contentIn this article
- Signs you should take your child to a doctor for a fever
- When to see a doctor for your child’s fever
- Common illnesses that can lead to fevers in children
- Uncommon illnesses that can lead to fevers in children
- At-home treatment for lowering your child’s fever until you can see a doctor
- How to get accurate readings for a child’s temperature
- How Doctor On Demand can assist when your child has a fever
- Doctor-answered FAQs for children’s fever
A fever in children can be part of a normal illness or a sign of a more serious issue. While uncomfortable, a fever is a normal part of the body’s defense system. This guide helps you recognize deeper concerns and make confident healthcare decisions.
Signs you should take your child to a doctor for a fever
Contact a doctor immediately if your baby is younger than 3 months and develops a fever. For older children, seek medical advice if the fever persists beyond a day or two, or sooner if they exhibit concerning symptoms, such as unusual drowsiness, labored breathing, seizures, rash, or vomiting.
Knowing when to worry about your child’s fever isn’t always straightforward. Factors such as your child’s age, how long the fever has lasted, and whether other symptoms are present all play a role. As noted in the 2017 article “Fever in Children: Pearls and Pitfalls“ from the National Library of Medicine states, “In most cases, fever is not dangerous and helps the body fight infection.”
Pay close attention to how your child is acting. Reach out to a healthcare provider if the fever persists for several days, climbs above 104°F, or is accompanied by symptoms such as difficulty breathing, severe fatigue, persistent vomiting, or an unusual rash. Trust your instincts and check in with your pediatrician when in doubt, even if symptoms seem mild.
What temperature is too high for a child with a fever?
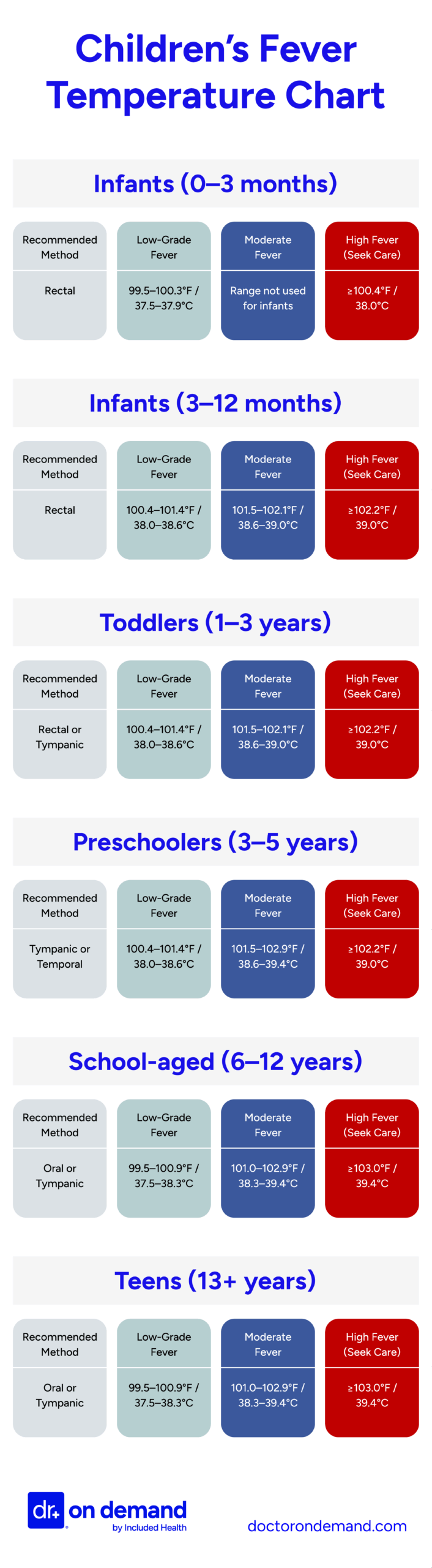
What counts as a concerning fever depends on your child’s age. While most fevers begin at 100.4°F (38°C), higher temperatures may require medical attention sooner in some age groups than others. Pediatricians often use the following rectal temperature thresholds as general guidance for what constitutes a high fever:
- Infants (0–3 months): 100.4°F (38.0°C) or higher
- Infants (3–12 months): 102.2°F (39.0°C) or higher
- Toddlers (1–3 years): 102.2°F (39.0°C) or higher
- Preschool-aged children (3–5 years): 102.2°F (39.0°C) or higher
- School-aged children (6–12 years): 103°F (39.4°C) or higher
- Adolescents (13 years and up): 103°F (39.4°C) or higher
Remember that a child’s behavior is as important as the number on the thermometer. A lower fever in a very young baby can be more serious than a higher fever in an older child who seems otherwise well.
How long should your child have a fever before seeing a doctor?
Babies under 3 months should be evaluated immediately for fever of 100.4°F (38°C) or higher. If your child is between 3 months and 2 years, contact a doctor if the fever lasts longer than 24 hours and is above 102.2°F (39°C). For children older than 2, see a doctor if the fever lasts more than 72 hours.
Young infants are especially vulnerable to serious infections, so even a mild fever requires immediate medical attention. In toddlers and preschoolers, fever lasting more than a day without improvement may need further evaluation, especially if no clear cause exists.
Symptoms that could mean your child’s fever needs medical attention
When paired with a fever, certain symptoms may signal a more serious problem requiring medical attention. These include breathing trouble, seizures, a stiff neck, constant vomiting or diarrhea, unusual drowsiness, a rash that doesn’t fade when pressed, or signs of dehydration like a dry mouth or fewer wet diapers.
Watch for the following warning signs:
- Unusual sleepiness or poor responsiveness: If your child is hard to wake, seems confused, or doesn’t respond normally, seek medical care right away.
- Breathing problems: Fast, labored, or noisy breathing can indicate a need for urgent attention.
- Ongoing vomiting or diarrhea can lead to dehydration and may point to an infection requiring treatment.
- Seizures: Any seizure, particularly one lasting longer than five minutes, should be evaluated immediately.
- Severe headache or stiff neck: When these occur with fever, they could suggest a more serious condition affecting the brain or spine.
- Unusual rash: If the rash doesn’t lighten when pressed or looks like bruising, contact your doctor immediately.
- Dehydration signs: These include a dry mouth, no tears when crying, and very few wet diapers or bathroom trips.
Children at higher risk for serious fever complications
Children at higher risk for serious fever complications include infants under 3 months old, children with chronic medical conditions, immunocompromised children, unvaccinated children, and those with a history of febrile seizures.
Children at increased risk for complications should be monitored closely and referred to a medical professional when they have high fevers. Below is a list of circumstances that warrant taking extra precautions:
- Infants under 3 months: Due to immature immune systems, they are more susceptible to serious infections and should be seen immediately for fevers over 100.4°F.
- Children with chronic medical conditions: Those with heart disease, lung disease, or other chronic illnesses may experience more severe effects from infections.
- Immunocompromised children: Children undergoing chemotherapy, taking immunosuppressive medications, or with conditions like HIV are at higher risk and should be seen for any high fever.
- Unvaccinated children: Unvaccinated children are more vulnerable to normally preventable diseases that can cause serious fever-related illnesses.
- Children with a history of febrile seizures: They may be more prone to recurrent seizures during febrile (fever) episodes.
When to see a doctor for your child’s fever
If your baby is under 3 months and has a fever over 100.4°F, contact a doctor immediately. A virtual visit can help for mild symptoms. Head to the ER or call 911 if your child has serious symptoms like trouble breathing, a seizure, or a rash that looks unusual.
When to take your child to their primary care doctor or pediatrician for a fever
Take your child to their primary care doctor or pediatrician if they are under 3 months old and have a fever over 100.4°F. For children 3 months to 2 years, see a doctor if the fever lasts more than 24 hours. For older children, seek care if a fever lasts more than 72 hours.
- Infants under 3 months: For babies younger than 3 months, a fever over 100.4°F should be checked out by a doctor right away, since they’re at higher risk for serious illness
- Children aged 3 months to 2 years: Kids between 3 months and 2 years should see a doctor if the fever lasts more than a day.
- Children over 2 years: For older children, get medical advice if the fever sticks around for more than three days or worsens.
When you can use telehealth for your child’s fever
You can use telehealth for your child’s fever if they are otherwise generally well and are not showing signs of serious illness. Telehealth is a good option for discussing symptoms, receiving treatment guidance, and determining whether a doctor’s visit is necessary.
Telehealth is a valuable tool that can help parents and caretakers determine the severity of a fever and whether accompanying symptoms warrant further medical care. Telehealth can effectively manage common pediatric conditions, including fevers, particularly when physical examination findings are not critical to immediate decision-making.
Telehealth professionals will want as much information about the child’s overall health and current condition as possible to determine the next steps in the child’s medical care.
When to take your child to urgent care for a fever
Take your child to urgent care if they have a fever and mild to moderate symptoms, especially if their regular doctor isn’t available. It’s a good option for non-emergencies like a lingering fever, sore throat, ear pain, or possible flu or strep throat.
Urgent care clinics are often an appropriate treatment option for children with fevers who may need further evaluation for underlying causes or illnesses.
When to go to an ER if your child has a fever
Go to the ER if your child has a fever and serious symptoms like trouble breathing, a stiff neck, a seizure, extreme drowsiness, or a rash. You should also seek emergency care if a high fever (over 102°F) lasts more than 48 hours without improvement.
When to call 911 if your child has a fever
Call 911 if your child has a fever and shows life-threatening symptoms such as a seizure lasting more than 5 minutes, severe difficulty breathing, or if their lips or face appear blue. These signs require immediate emergency medical attention.
Most fevers in children are not life-threatening and resolve themselves once the underlying cause is treated. However, there are rare conditions that warrant calling 911 for immediate care.
If a child with a fever has any life-threatening symptoms, such as a seizure lasting more than 5 minutes, difficulty breathing, or severe illness, you should call 911 immediately. Any time a child has trouble breathing or if their lips or face appear blue, you should call 911.
Common illnesses that can lead to fevers in children
Fevers in children are often caused by common infections such as the flu, COVID-19, hand, foot, and mouth disease, strep throat, and urinary tract infections. In most cases, treating the underlying illness helps bring the fever down as the child recovers.
Several common illnesses can lead to fevers in children:
- Influenza (flu): Children under the age of 5 are particularly susceptible to flu-related complications, which include high fever, cough, sore throat, and muscle aches.
- COVID-19: COVID-19 can cause high fevers in children. Fever is a prevalent symptom of COVID-19 in children, often accompanied by respiratory symptoms.
- Hand, foot, and mouth disease (HFMD): A frequent viral illness in young children, HFMD often begins with a fever and is followed by painful sores in the mouth and a rash on the hands (palms) and feet (soles). It typically resolves on its own within a week to ten days without the need for medical treatment.
- Streptococcal pharyngitis (strep throat): Strep throat is a bacterial infection that causes sore throat and fever and is common in children.
- Urinary tract infection (UTI): UTIs can cause fever in children, and doctors may request urine testing when a UTI is suspected.
Uncommon illnesses that can lead to fevers in children
Uncommon causes of fever in children include Kawasaki disease, meningitis, rheumatic fever, autoimmune conditions like juvenile idiopathic arthritis, tick-borne illnesses such as Rocky Mountain spotted fever, and endocarditis. These rare illnesses may require testing to diagnose and treat appropriately.
- Kawasaki Disease: Kawasaki Disease is a rare inflammatory condition that primarily affects children under 5 years old, causing prolonged fever, rash, red eyes, swollen hands and feet, and cracked lips, and has emerged in children following COVID-19 infections.
- Meningitis: This serious illness involves inflammation of the tissues that cover the brain and spinal cord. It can be caused by either viruses or bacteria and often leads to symptoms like fever, a stiff neck, intense headache, light sensitivity, and extreme fatigue or sluggishness. Prompt diagnosis and treatment are critical.
- Rheumatic fever: This is a rare complication of untreated strep throat or scarlet fever, leading to fever, joint pain, rash, and heart inflammation.
- Autoimmune diseases: Conditions like juvenile idiopathic arthritis (JIA) or lupus can cause recurring fevers and joint pain, fatigue, or rashes.
- Rocky Mountain Spotted Fever: This tick-borne illness can cause fever, headache, rash, and muscle pain, though it is rare and geographically specific.
- Endocarditis: A rare infection of the heart’s inner lining, endocarditis can cause fever, fatigue, and heart-related symptoms.
At-home treatment for lowering your child’s fever until you can see a doctor
There are many at-home treatments to reduce a fever or make your child more comfortable until you can get medical care. While these treatments will not address the underlying causes of the fever, they can ease the discomfort that often comes with it.
- Ensure proper hydration: Encourage your child to drink plenty of fluids, such as water, clear broths, or electrolyte drinks, to prevent dehydration. For infants, continue breastfeeding or formula feeding.
- Use fever-reducing medications: Administer acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) as directed by your pediatrician or according to the dosage instructions based on your child’s age and weight. Avoid giving aspirin to children, as it can cause Reye’s syndrome (sudden brain damage and liver dysfunction).
- Dress lightly: Dress your child in lightweight clothing and avoid heavy blankets to help their body release heat.
- Provide a lukewarm bath: A lukewarm (not cold) bath can help bring down your child’s temperature. Avoid cold water or ice baths, as they can cause shivering and raise the body temperature.
- Use a cool compress: Place a cool, damp washcloth on your child’s forehead or the back of their neck to provide comfort. According to Dr. Ashley Kelley, a pediatrician at Included Health: “I always remind parents of my patients that the goal of these treatments is to increase comfort, not to resolve the fever. If the cool compress or lukewarm bath makes your child uncomfortable or causes crying, focus instead of rest, hydration, comfortable clothing and bedding.”
- Encourage rest: Make sure your child gets plenty of rest to help their body fight off the illness.
- Monitor their temperature: Check your child’s temperature regularly to track any changes and ensure it doesn’t rise too high.
- Medicines: Follow the correct dosing schedule for fever reducers, and consult your pediatrician if you’re unsure which medication is appropriate. Keep a log of when medications are given to avoid accidental overdosing.
- Sponging: If your child has a persistent fever, gently sponge their body with lukewarm water, focusing on areas like the armpits, neck, and groin. Stop if your child becomes uncomfortable or starts to shiver.
How to get accurate readings for a child’s temperature
There are four common ways to check a child’s temperature, each with varying degrees of accuracy and usefulness. Rectal temperature readings are the most accurate for infants and young children. As children get older, using ear (tympanic) temperature can yield accurate results. Forehead temperature is suitable for all ages of children and is non-invasive, so you can check your child’s temperature while they sleep.
“Getting an accurate temperature reading for a child is important to prevent unnecessary interventions as well as detect serious illness earlier in its course,” says Dr. Ashley Kelley. “When you contact your healthcare provider to discuss your child’s fever, they may ask how you checked the temperature, which helps your healthcare provider determine what treatment or action may be needed.”
Rectal temperature (Most accurate for infants and young children)
- When to use: Best for infants and children under 3 years old. Recommend a digital thermometer.
- How to measure:
- Clean the thermometer with soap and water or rubbing alcohol, then rinse with cool water.
- Apply a small amount of petroleum jelly to the tip of the thermometer for easier insertion.
- Lay your child on their back or stomach, holding them securely.
- Gently insert the thermometer about ½ to 1 inch into the rectum (never force it).
- Hold the thermometer in place until it beeps, then remove and read the temperature.
- Normal range: 97.9°F to 100.4°F (36.6°C to 38°C).
Ear (tympanic) temperature
- When to use: Suitable for children over 6 months old.
- How to measure:
- Use a clean, properly fitted ear thermometer.
- Gently pull the ear back and up (for children over 1 year) or straight back (for children under 1 year) to straighten the ear canal.
- Insert the thermometer into the ear canal and press the button to take the reading.
- Ensure the thermometer is positioned correctly for an accurate result.
- Normal range: 96.4°F to 100.4°F (35.8°C to 38°C).
Forehead (temporal artery) temperature
- When to use: Non-invasive and suitable for all ages.
- How to measure:
- Use a temporal artery thermometer.
- Place the thermometer on the center of your child’s forehead.
- Slowly move it across the forehead toward the temple or hairline, following the manufacturer’s instructions.
- Some thermometers may require you to press a button while scanning.
- Normal range: 97.9°F to 100.1°F (36.6°C to 37.8°C).
Armpit (axillary) temperature
- When to use: Easy to use but less accurate; often used as a quick screening method.
- How to measure:
- Place the thermometer under your child’s armpit, ensuring it touches the skin (not clothing).
- Hold your child’s arm snugly against their body to keep the thermometer in place.
- Wait until the thermometer beeps, then read the temperature.
- Normal range: 97.8°F to 99.5°F (36.5°C to 37.5°C).
How Doctor On Demand can assist when your child has a fever
If your child has a fever and you need answers fast, start a virtual visit with a board-certified provider today through Doctor On Demand. Whether the fever is mild or persistent, our 24/7/365 virtual care gives you quick access to expert guidance—all from the comfort of home.
Doctor On Demand providers can help you determine what’s causing the fever and whether your child may need further evaluation. If appropriate, they can prescribe medications such as antibiotics or fever reducers and send them directly to your preferred pharmacy. They can also walk you through safe, effective at-home care using over-the-counter treatments. During your visit, the provider will:
- Assess your child’s symptoms: You’ll discuss how high the fever is, how long it’s lasted, and whether your child has other symptoms like a rash, sore throat, cough, or decreased appetite.
- Identify the likely cause: Your doctor will evaluate whether the fever is most consistent with a viral illness (like the flu or hand, foot, and mouth), a bacterial infection (like strep throat or a UTI), or another condition.
- Recommend next steps: Get clear guidance on managing the fever at home, whether prescription treatment is needed, and when to follow up with in-person care.
While many childhood fevers can be safely managed through a virtual visit, your doctor will let you know if your child needs to be seen in person or requires further testing. If your child’s symptoms raise concern, your provider will explain what to do next.
Want fast, expert care for your child’s fever? Sign up for Doctor On Demand and connect with a board-certified provider in minutes.
How to prepare for your Doctor On Demand Visit
A virtual visit with Doctor On Demand is fast, convenient, and designed to fit your schedule. To help your provider give the best care possible when your child has a fever, a few simple steps can make your visit even smoother.
Choose a quiet, well-lit space: Find a calm spot in your home with good lighting so your doctor can see and hear you clearly during the video call. If your child will be present for the visit, make sure they’re comfortable and easy to observe.
Take notes on your child’s symptoms: Before the visit, jot down a few details about your child’s fever, such as:
- When did the fever start, and has it gone up or down?
- Are there any other symptoms, such as a cough, rash, sore throat, fatigue, or decreased appetite?
- Have they been exposed to anyone who’s been sick recently?
Have a thermometer ready: A recent temperature reading is one of the most helpful tools for your provider. If you also have a pediatric pulse oximeter, keep it nearby. Additional lighting, like a lamp or smartphone flashlight, may help if your doctor wants to examine your child’s skin, throat, or breathing.
List any medications or health history: Be prepared to share what prescription or over-the-counter medications your child is currently taking. Mention any recent diagnoses or ongoing health conditions as well.
Bring your questions: Whether you’re unsure about medication, home remedies, or when to seek in-person care, write down your questions so you don’t forget anything during the visit.
Taking a few moments to prepare can help you and your Doctor On Demand provider make the most of your time—and get your child on the path to feeling better, faster.
Doctor-answered FAQs for children’s fever
This FAQ answers common questions about childhood fever, including what temperature counts as a fever, when to be concerned, and how to treat a fever at home. You’ll also learn when it’s safe to let a fever run its course and when to call a doctor.
What counts as a fever in a child?
A fever in a child is generally defined as a body temperature that is higher than normal. The specific threshold for a fever depends on the method used to measure the temperature. Here are the general guidelines:
- Rectal temperature: A fever is considered 100.4°F (38°C) or higher. This is the most accurate method for infants and young children.
- Oral temperature: A fever is considered 100°F (37.8°C) or higher.
- Ear (tympanic) temperature: A fever is considered 100.4°F (38°C) or higher.
- Forehead (temporal artery) temperature: A fever is considered 100.4°F (38°C) or higher.
- Armpit (axillary) temperature: A fever is considered 99°F (37.2°C) or higher, though this method is less accurate.
When should I be concerned about my child’s fever?
Be concerned about any fever if your child is under 3 months old, if fever lasts more than 3 days in older children, or if it comes with serious symptoms like trouble breathing, seizure, rash, vomiting, or extreme fatigue. Always seek care if your child seems unusually sick or “off.”
Fever concerns depend on your child’s age, how long the fever lasts, and what other symptoms appear. Infants under 3 months need immediate care for any fever over 100.4°F. For older children, look out for high fever that doesn’t improve, difficulty waking, or signs of dehydration like no urination or dry mouth.
Why is a fever sometimes considered good in a child?
Fever is often a good sign in children—it means their immune system is responding to infection. A higher temperature helps slow the growth of viruses and bacteria and activates immune defenses. Most childhood fevers are short-lived and help the body fight off illness naturally.
What to do if my child’s only symptom is a fever?
If your child has a fever but no other symptoms, you can usually monitor them at home. Keep them comfortable, hydrated, and rested. Use fever medicine only if they’re uncomfortable. For babies under 3 months, see a doctor right away. For older kids, call the doctor if the fever lasts over 3 days.
While most fevers in children are caused by minor viral illnesses, it’s important not to overlook the possibility of something more serious, especially when there’s no obvious source. A 2000 report titled “Management of Fever Without Source in Infants and Children” from the University of California’s Department of Pediatrics and Emergency Medicine explains that “most febrile illnesses in children are benign and self-limited, but a small percentage are caused by serious bacterial infections.” Recurrent or unexplained fevers, particularly in younger children, should be discussed with a doctor to rule out underlying issues.
What can cause unexplained fevers in children?
Unexplained fevers in children are often early signs of viral infections such as roseola or enterovirus. Other causes include urinary tract infections, sinus infections, or reactions to vaccines. Persistent or recurring fevers may signal autoimmune conditions, bone infections, or rarely,certain cancers. A doctor can help identify the cause if the fever continues.
When can children return to school after having a fever?
Children can return to school when they’ve been fever-free for at least 24 hours without using fever medicine and are clearly feeling better. If the fever was from a contagious illness like strep or COVID-19, follow your doctor’s or school’s return-to-school rules.
Should you let a child sleep with a fever?
Yes, you can let your child sleep when they have a fever—rest is important for recovery. Just check in on them now and then to make sure they’re doing okay. Dress them lightly, avoid heavy blankets, and make sure they’re drinking fluids when they wake up.
How often should you check a child’s fever at night?
You don’t need to wake your child just to check their fever if they’re sleeping well and seem stable. For fevers over 102°F, consider checking every 4 to 6 hours. Use your judgment and watch for signs like fast breathing or unusual restlessness that may need closer monitoring.
What to do if my child’s fever won’t go down?
If your child’s fever won’t go down, confirm the temperature with a reliable thermometer. Give acetaminophen or ibuprofen in the correct dose for their age and weight. Keep them hydrated, lightly dressed, and in a cool room. Call a doctor if serious symptoms appear or the fever persists without improvement.
If they start having trouble breathing, develop a bad headache or stiff neck, get a rash that looks like bruises, vomit or have diarrhea that won’t stop, seem confused or very tired, or aren’t peeing, it’s time to call the doctor.
When should I let my child’s fever run its course?
If your child is older than 3 months, has a fever under 102°F and seems comfortable—eating, drinking, and acting mostly like themselves—it’s usually fine to monitor without medication. Fever plays a helpful role in fighting off infection and doesn’t always need treatment right away.
Let the fever be if:
- Your child is alert, resting well, or playing quietly.
- There are no concerning symptoms like difficulty breathing, an unusual rash, or signs of dehydration.
- The fever is short-lived, lasting two or three days or less.
- Your child doesn’t seem distressed by the fever itself.
In these situations, focus on keeping them hydrated and rested. Fever-reducing medicine is optional and can be used if the fever makes your child uncomfortable.
About the authors

Dr. Jeanette Carpenter is board certified in Family Medicine and practices in Virginia. She has an interest in preventative medicine and holistic medicine and has a certification in plant based nutrition from eCornell. She believes stress and lifestyle impacts the disease process and spends extra time educating patients on lifestyle modifications that can improve their overall health.

Quan Lam is a copywriter with over 15 years of experience writing and editing content for both start-ups and legacy brands, as well as 2 years of writing experience exclusively within the healthcare space. She currently lives and works in New York City.



