Table of contentIn this article
- When to go to the ER for vomiting
- Recognizing vomit color and types to assess seriousness
- Symptoms that indicate vomiting may be serious
- What can a hospital ER do for your vomiting
- From mild to serious, what can trigger or cause vomiting
- How can you treat mild vomiting at home?
- How Doctor on Demand can assist with your vomiting
- Doctor-answered FAQs for vomiting
Vomiting often stems from a mild issue, like an infection or bad food. But sometimes, it signals a problem that needs urgent care. Learn which symptoms require an ER visit, what doctors can do, and how to manage mild cases at home or through telehealth.
When to go to the ER for vomiting
Go to the ER if vomiting comes with red flags like severe belly pain, an intense headache, confusion, or blood in your vomit. These symptoms could point to a serious underlying issue. Also, seek care if you’re vomiting so often that you feel severely dehydrated.
If you are vomiting and develop any of the following symptoms, or it feels very serious, don’t wait–go to the ER:
- Your vomit is red or very dark.
Bright red vomit, or black vomit that resembles wet coffee grounds, indicates that you have blood in your vomit. Usually, this is caused by bleeding in your upper gastrointestinal (GI) tract, such as the esophagus, stomach, and duodenum. An upper GI bleed can become a life-threatening situation without immediate care—go to the ER.
- You are confused or have a strong headache.
Vomiting paired with neurological symptoms, such as feeling confused or having a strong headache, is a serious red flag. It may point to a serious problem in the brain itself, such as head injury, meningitis (brain infection), or even a stroke.
- You have serious chest pain or an irregular heartbeat.
If your heart isn’t pumping properly, it can reduce blood flow to the stomach and trigger nausea or vomiting. When vomiting occurs alongside chest pain, shortness of breath, or a racing or irregular heartbeat, it may signal a cardiovascular issue, such as a heart attack.
- You have intense abdominal pain.
If you experience severe, unrelenting, or localized abdominal pain, you might have internal bleeding, a bowel obstruction, appendicitis, pancreatitis, or another condition, all of which require immediate care. If you also haven’t passed stool in a few days, you may have a bowel obstruction that needs emergency care.
- You can’t keep fluids down.
If you can’t hold down even sips of water and your vomiting continues for more than a day, you’re at risk for severe dehydration, which itself can be dangerous. Signs of intense dehydration include passing only small amounts of urine infrequently, having dark yellow urine, having a rapid heart rate, and having dry skin or a dry mouth. If you have these signs or can’t hold down liquids for more than a day or two, go to an ER.
- Your vomiting has lasted more than 48 hours, and it’s not getting better.
If you’re vomiting frequently and it’s not getting better within two days, it’s wise to go to the ER even if you don’t have any of the red-flag symptoms yet.
- You have a high fever.
If you have a high fever (~102 °F and above), you might have a bacterial infection or a systemic infection like sepsis. If you also have diarrhea, it might be a sign of bacterial gastroenteritis or even a parasitic infection.
You have known risk factors.
If you have cancer, diabetes, recent surgery, or new medications, and your vomiting doesn’t seem like a simple stomach bug, go to the ER. Also, go to the ER if you suspect you’ve ingested something potentially toxic or that you’re allergic to.
When to call 911
Call 911 if you are too ill to safely get to the ER on your own or if your symptoms suggest a life-threatening emergency. If you’re experiencing sudden confusion, extreme shortness of breath, or intense abdominal pain, don’t wait. Calling 911 could save your life.
If you or someone nearby is experiencing complex or rapidly worsening symptoms along with vomiting, it could be a life-threatening emergency. These situations often overlap with the criteria to go to the ER, but they tend to come on more suddenly and feel more intense. Paramedics can begin critical care on the way to the hospital, and in many cases, that early intervention can be life-saving.
Call 911 if you’re facing any of the symptoms or situations below and aren’t confident you can get to the ER safely:
- Potential loss of consciousness
If you’re vomiting and drifting in and out of consciousness, you’re at risk of choking on your vomit. If vomit enters the lungs, it can block breathing or cause life-threatening complications. This is a medical emergency—call 911.
- Severe neurological symptoms
If you or someone else is experiencing facial drooping, blurred vision, double vision, difficulty speaking, and high blood pressure (hypertension), it might indicate a stroke or another severe neurological issue.
If you have these symptoms alongside projectile vomiting, meaning you’re vomiting so forcefully that you can “project” your vomit, you might have increased intracranial pressure (an increase in pressure in your skull). This condition can be from a stroke, brain hemorrhage, brain tumor, meningitis, or something else. Call 911.
- Severe cardiovascular symptoms
If your vomiting comes with sudden and intense chest pain, a racing or irregular heartbeat, or arm pain, it could signal a cardiovascular emergency like a heart attack or an arrhythmia. These are time-sensitive conditions where every minute counts.
- You can’t keep fluids down and are developing a fever.
Vomiting combined with persistent dehydration, high fever, lethargy, or inability to hold down fluids for over 12 hours may indicate a serious systemic problem like sepsis, a kidney infection, or even toxic shock. If you’re getting weaker or more confused, or you can’t sit up without feeling faint, call 911.
- Suspected poisoning or overdose
If you think you or someone else may have ingested a harmful substance, call 911 immediately. The symptoms of poisoning or an overdose can escalate quickly, and most antidotes are very time sensitive and need to be administered as soon as possible to be effective. First responders can administer these and other life-saving interventions en route. Alongside vomiting, signs of dangerous poisoning can include trouble breathing, large pupils, and even a seizure.
- You hit your head and began vomiting later.
If you or someone has hit their head and later begins vomiting, it might be a sign of a brain bleed that needs immediate care. Don’t hesitate to call 911, especially if the symptoms are severe and escalating rapidly.
- Your instincts say something is very wrong.
In general, call 911 if you feel too ill to get to the ER safely or if your gut feeling is telling you something is very wrong. Trust your instincts.
When you can use telehealth for vomiting
Telehealth is a good option if you want relief from mild vomiting symptoms that you suspect are food poisoning or a stomach bug. It’s helpful if you feel sick but just need advice for home care or a prescription. If you develop serious symptoms, go to the ER.
In today’s world, virtual telehealth visits can be a convenient first step for mild cases of vomiting. A doctor can evaluate your symptoms remotely, offer treatment advice, and prescribe medications to help. In fact, telehealth is ideal for mild cases because you can avoid waiting in a sitting room while you feel sick or are potentially contagious, but still receive professional advice.
However, telehealth is not meant for emergencies. If your symptoms are severe—or you think your vomiting might be related to something more serious than a stomach bug—go to the ER or call 911 right away.
Here’s when using telehealth to manage vomiting is appropriate:
- You’re experiencing mild or moderate vomiting.
If your symptoms are uncomfortable but manageable, a virtual visit can help you get relief without leaving home. For example, if you had a rough night of vomiting from what you think is food poisoning or a stomach bug, but you’re starting to feel better, you can talk to a virtual urgent care doctor to help you with next steps.
- You suspect the stomach bug.
The stomach bug, also known as stomach flu (gastroenteritis), is one of the most common causes of intense but short-term vomiting. A telehealth provider can confirm that it’s likely gastroenteritis and guide you through home care.
- You suspect food poisoning or an allergy.
If you recently ate something suspicious or new and now have vomiting, but no other severe symptoms, telehealth is a good starting point for care.
- Your vomiting is chronic but mild, or triggered by a specific event or food.
If your vomiting is a recurring issue, for example if you notice you vomit after certain foods or sometimes after a medication, you don’t need to rush to the ER. A virtual visit with your primary care physician can help you get to the bottom of your situation.
- Vomiting during pregnancy (morning sickness)
If you are pregnant and experiencing typical morning sickness (where you can hold some food and fluids down), you can use telehealth to explore potential remedies with your doctor.
- You don’t have any red flag symptoms.
Telehealth is reasonable if you have no signs of severe pain, bleeding, dehydration, or neurological symptoms like confusion or weakness. If anything changes, though, you may still need in-person follow-up.
When to wait and see your primary care doctor
See your primary care doctor if your vomiting is mild, comes and goes, and you suspect it’s linked to a chronic issue like food intolerance or a medication side effect. Your primary doctor can help identify the cause or refer you to a specialist for further evaluation.
In these cases, your doctor can help figure out what’s causing your symptoms and offer a long-term plan to manage or prevent them. They can also refer you to a specialist if needed and help you monitor for patterns or triggers over time.
That said, if you’re vomiting uncontrollably, unable to stay hydrated, or have a strong sense that something’s wrong, go to the ER instead. But if your symptoms are stable and you’re searching for answers, your primary care provider is a good place to start.
Here’s when it’s safe to wait to see your primary care doctor about vomiting:
- Your vomiting is mild, intermittent, and you can keep fluids down.
If you’re only vomiting now and then, and it’s not intense, and you have no other serious symptoms, it might be linked to a chronic issue like acid reflux. In these cases, it’s usually safe to wait and talk to your primary care doctor to figure out what’s going on.
- You’re not experiencing any red-flag symptoms.
If you don’t have any red-flag symptoms, it’s probably safe to wait for your primary care doctor. But if you develop any signs of severe pain, bleeding, confusion, a high fever, or neurological symptoms, seek ER care.
- You suspect a chronic issue that comes from a specific trigger.
If you suspect that your symptoms are from something like acid, a food allergy or intolerance, medication side effects, or another ongoing condition, it’s best to speak with your primary doctor. They can help narrow down the causes or refer you to a specialist.
- You need a referral for long-term management.
If you’ve already been treated in the ER and now need follow-up care, your primary doctor can help coordinate next steps or refer you to a specialist.
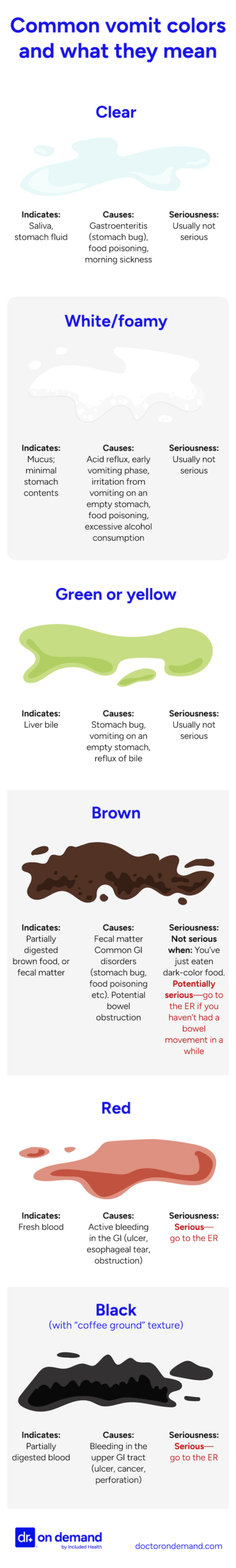
Recognizing vomit color and types to assess seriousness
The color of your vomit can offer clues about its cause and severity, especially alongside other symptoms. Clear, white, green, and yellow vomit is usually not serious. Red, dark brown, or black vomit means you have blood in your vomit and you need urgent care.
The color and appearance of vomit can offer important information about what’s causing your vomiting, but experts agree that vomit color alone usually isn’t enough to make a diagnosis. Other symptoms matter just as much, if not more.
Here’s a list of common vomit colors and what they might indicate about your condition. Even if your vomit color indicates a “mild” condition, go to the ER if you start experiencing red-flag symptoms, such as confusion, severe pain, or dizziness.
The following colors of vomit usually aren’t serious, unless they’re paired with other symptoms:
- Clear or whitish vomit:
On its own, clear, whitish vomit is usually not a serious sign.
Clear vomit is usually saliva or stomach lining fluid that comes when you vomit on an empty stomach. If you’ve been vomiting repeatedly without eating, this is common and not usually serious.
“As an urgent care physician, it was not uncommon for me to see pediatric cases where the child was vomiting up mostly clear mucus because they had a cold with significant post-nasal drainage and that was irritating the stomach. Children are particularly prone to vomiting due to post-nasal drip because they may not be as adept at clearing the mucus through coughing or blowing their noses, leading to more swallowing of the mucus.” add MD name here
One exception: It’s worth noting that if someone has had head trauma and begins vomiting, the vomit is usually white or clear. So if you have clear vomit and recently hit your head, it’s a serious situation due to the head injury, not the vomit color itself.
- White and foamy vomit:
White, foamy vomit is typically caused by irritation of the stomach lining, often from gastritis (inflammation of the stomach lining), acid reflux, or excessive alcohol. It may also appear after eating certain foods. Usually, it’s not serious.
- Yellow or green:
Yellow or green vomit is usually bile, a fluid your liver produces. Yellow is digested bile, and green is undigested bile. Usually, vomiting bile isn’t serious, especially if you’ve been vomiting on an empty stomach.
One exception: If yellow or green vomit comes with other symptoms, particularly severe abdominal pain, it may point to dehydration, acid reflux, gastritis, or an intestinal blockage that should be evaluated.
The following colors of vomit can indicate:potentially serious conditions:
- Brown:
Brown vomit is often harmless and is usually just the color of food you’ve recently eaten. But it can sometimes indicate a bowel obstruction, especially if it smells like feces.
- When it’s usually not serious
- You’ve recently eaten something dark, such as chocolate or dark-colored sauces.
- You don’t have other symptoms like severe pain or neurological changes.
- When it might be serious and require attention
- You haven’t had a bowel movement in several days and you have fecal-smelling vomit. This situation is uncommon, but pressing. In the 2007 review “Evaluation of Nausea and Vomiting,” published in American Family Physician, the authors note that fecal-smelling vomit is very rare, but it can happen with an intestinal obstruction. In this case, seek medical care immediately.
- You haven’t had a bowel movement in several days and you have fecal-smelling vomit. This situation is uncommon, but pressing. In the 2007 review “Evaluation of Nausea and Vomiting,” published in American Family Physician, the authors note that fecal-smelling vomit is very rare, but it can happen with an intestinal obstruction. In this case, seek medical care immediately.
- Orange:
- Usually, orange vomit is from partially digested food that was in your stomach.
- When it’s usually not serious
- You’ve eaten recently, and the vomit has food particles.
- You don’t have other red-flag symptoms.
- When it might require attention
- Orange vomit continues on an empty stomach suggests a bile reflux. If orange vomit becomes more redredder, it could signal bleeding higher in the GI tract.
- It’s paired with dehydration or signs of obstruction.
The following colors of vomit that unequivocally signal a serious problem:
- Bright red, bloody:
Bright red vomit is from fresh blood (hematemesis). If you even have a small amount of blood in your vomit, it likely indicates active bleeding in the upper part of your digestive tract. Common causes include bleeding stomach ulcers, esophageal tears (like a Mallory-Weiss tear, often from repeated vomiting), or esophageal varices (engorged blood vessels in the wall of the esohagus). There is no doubt among experts that red vomit signals a medical emergency that needs immediate care.
- Dark red “coffee grounds” vomit:
If your vomit looks like wet coffee grounds, it means that you’ve had blood in your stomach long enough that it’s been partially digested by your stomach acid. Like red vomit, dark red vomit means you have an upper GI bleed, though it might be slow or has stopped. All doctors will treat “coffee ground” emesis as an upper GI bleed that needs critical care.
- Black vomit:
Like dark red blood, black vomit that resembles coffee grounds often means you have partially digested blood in your stomach. It can signal internal bleeding, often from a peptic ulcer, a tumor, or even liver failure (especially in people with cirrhosis). Doctors sometimes refer to this as “coffee ground emesis.” Always get medical attention for black or very dark vomit.
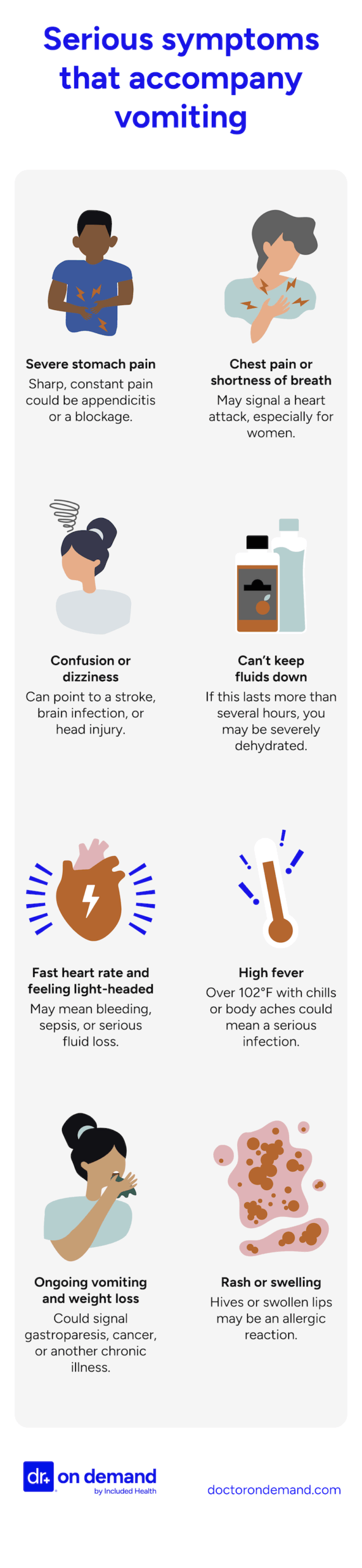
Symptoms that indicate vomiting may be serious
Vomiting may be serious if it comes with severe pain, shortness of breath, a strong headache, or a sense that something is very wrong. It’s also concerning if you can’t keep fluids down for more than a day. These and other red-flag symptoms warrant urgent medical attention.
In The American Journal of Gastroenterology’s 2021 review, “Nausea and Vomiting in 2021: A Comprehensive Update,” the authors note that there are many symptoms that might signal vomiting is more than a passing illness. According to the article, key red-flag symptoms include severe abdominal pain, fever, and any neurological changes, such as dizziness or confusion. The authors also suggest seeking care immediately if you can’t keep fluids down at all or if you have blood in your vomit.
Here’s a comprehensive list of symptoms beyond what your vomit looks like that should raise concern, especially if they come on suddenly or don’t improve:
- Severe abdominal pain
Unrelenting, severe stomach pain that is sharp, stabbing, or constant warrants going to the ER immediately. This symptom might be from appendicitis, pancreatitis, or an internal blockage. In particular, pain that precedes vomiting, or is localized (like to the right lower abdomen, common in appendicitis), might signal a condition that needs emergency surgery to treat.
- Chest pain, shortness of breath, and/or arm and shoulder pain
Chest discomfort along with vomiting may point to heart problems (like a heart attack), especially in older adults. Especially for women, this often comes with arm pain, shoulder pain, jaw pain, or a stiff neck. Even if it’s just mild pain, it should be taken seriously.
- Neurological signs
Your brain receives signals from the gut and triggers vomiting as a protective reflex to expel harmful substances. But sometimes, that system misfires and your brain may tell your body to vomit even when there’s no real threat.
That’s why vomiting combined with confusion, dizziness, blurred vision, slurred speech, or difficulty walking or staying awake is among the most troubling combinations of symptoms. They can point to a brain-related issue like a head injury, stroke, or brain infection.
- Signs of severe dehydration, such as shock
If you can’t even sip water without vomiting for more than several hours, you’re at risk of becoming very dehydrated. Signs include urinating very infrequently, having dark urine that smells strongly, and feeling lightheaded when you stand up.
- High heart rate
A rapid heart rate, especially if you’re also feeling lightheaded, can be a sign of a serious systemic issue. When it happens alongside vomiting, it may point to internal bleeding, severe dehydration, or a serious infection like sepsis. Seek medical care right away.
- High fever with signs of a systemic infection
A high fever alongside vomiting may signal a more serious infection. It’s especially concerning if it’s high (over 102°F), keeps climbing, or is paired with body aches, chills, fatigue, or a high heart rate. It could indicate a serious infection, such as sepsis or meningitis.
- Persistent vomiting paired with weight loss and fatigue
If you have been vomiting off and on for weeks and you notice you’re losing weight or not getting better, it could mean your body is struggling with something more complex than a simple stomach bug. For example, conditions like gastroparesis (delayed stomach emptying, common in people with type 1 diabetes) or some types of cancer can cause persistent vomiting with weight loss.
- Rashes, swelling, or other signs of an allergic reaction
If you’re vomiting and also develop swelling of your lips and tongue, hives, or a rash, you might be having a severe allergic reaction.
Symptoms of becoming dehydrated from vomiting
When you vomit repeatedly, your body loses fluids fast and you’re at risk of becoming severely dehydrated, which can be an emergency. Signs of dehydration include urinating less often, very dark urine, dry skin, and reduced skin elasticity. You might also feel lightheaded or get muscle cramps.
Severe dehydration can happen quickly when you’re vomiting and unable to keep fluids down. You can become very dehydrated even if the underlying cause of your vomiting isn’t serious. One of the earliest signs of dehydration is increased thirst, your body’s signal to replace lost fluids. If you’re feeling unusually thirsty, it’s a sign to begin rehydrating as soon as possible. Mild dehydration usually gets better with home care, as long as you can keep fluids down. Even small sips of water at a time can be enough.
But if you begin to feel severely dehydrated, you may need to go to the ER for IV fluids to restore your hydration and electrolyte balance quickly.
Here’s a list of dehydration symptoms to watch out for:
- You’re not urinating often, or your urine is very dark.
If you’re urinating less often than usual—or only passing a small amount each time—it likely means you’re dehydrated. Very dark yellow or amber-colored urine, especially if it has a strong smell, is a common sign that your body is low on fluids.
- Elevated heart rate and low blood pressure (hypotension)
When you lose too much fluid, your heart works harder to circulate what’s left. This can lead to a rapid heart rate. At the same time, your blood pressure may drop, a condition called hypotension, making you feel dizzy, light-headed, or faint when standing up. Alongside vomiting, these are clear signs of severe dehydration. Seek medical care immediately.
- Your skin is dry and has poor turgor.
Dehydrated skin often feels dry and less elastic. If you gently pinch the skin on the back of your hand and it doesn’t snap back quickly, you may be dehydrated. You might also notice dryness in the mucus membranes in your mouth, lips, eyes, and nose.
- Headache, weakness, confusion
If you begin to feel unusually weak, foggy, or mentally confused, you may be severely dehydrated, and you should go to the ER immediately.
- Muscle cramps
Vomiting doesn’t just deplete water. It also causes an electrolyte imbalance that causes your muscles to spasm. If you’re experiencing severe cramps, spasms and muscle twitching alongside vomiting, it’s likely that you’re low on both fluids and electrolytes.
What can a hospital ER do for your vomiting
At the ER, doctors check for serious causes of your vomiting. They may give you IV fluids and anti-nausea medicine to help you feel better. If needed, they’ll treat the cause, monitor you, and decide whether you need to stay in the hospital or go home.
In the 2008 review article “The Vomiting Patient in the ED: Evaluation and Management” from the journal Emergency Medicine Reports, the authors explain that the first job of ER doctors is to make sure the vomiting isn’t a sign of something life-threatening—like appendicitis, meningitis, or sepsis. Then, the authors break down the next steps: ER doctors also check for severe dehydration and signs of a blockage in the digestive tract. Lab tests can help, but the main goal is to figure out if the problem might need surgery. If not, and the patient starts to feel better, they may be treated with medication and sent home. However, if the vomiting is extreme or suggests a more serious condition, the patient may need to stay in the hospital for further care.
Here’s what you can expect if you go to a hospital ER for vomiting:
- Diagnostic evaluation
First, the staff will identify any red flags, like neurological signs or abdominal pain, to determine quickly how severe and urgent your situation is. They’ll focus on ruling out emergency causes like bowel obstruction or pancreatitis.
Based on their initial diagnosis, they might order lab tests to identify whether you have an infection, you’re dehydrated, or have any other metabolic issues. If they suspect that your GI tract is obstructed or perforated, they might perform rapid imaging, such as an ultrasound.
- Aggressive fluid resuscitation and antiemetic medication
If they suspect cyclic vomiting syndrome (CVS), or if you’ve been vomiting frequently, you’ll receive IV fluids and antiemetic medication like ondansetron and haloperidol.
In the previously mentioned article “The Vomiting Patient in the ED: Evaluation and Management,” the authors explain that ER doctors only use antiemetics to slow or stop vomiting that’s severe, harmful, or not improving on its own. That’s because the medications themselves can have troublesome side effects like sedation, movement disorders, or heart rhythm changes, especially in people with certain pre-existing conditions. The authors stress that first-line medications, like Zofran, can help, but they only treat the symptoms, not the underlying cause.
- Treat the underlying cause
If your situation is urgent, ER doctors will order tests to diagnose and treat your underlying cause. For example, if you have an obstruction in your GI tract, you might receive emergency imaging and surgery. They might administer antibiotics or other medications tailored to your diagnosis.
- Monitoring & next steps
The staff will observe and track your response and discharge you if your symptoms improve with fluids and medications. They will admit you if you have a serious condition and need emergency treatment.
From mild to serious, what can trigger or cause vomiting
The most common mild causes of vomiting are stomach viruses and food poisoning, which usually resolve with rest and fluids. Moderate causes include food allergies, gut inflammation, and cyclic vomiting syndrome. Serious causes include GI obstruction, pancreatitis, poisoning, and some heart or neurological conditions.
Vomiting can be caused by anything from a mild stomach bug to a life-threatening emergency. In the 2008 article “The Vomiting Patient in the ED: Evaluation and Management” from Emergency Medicine Reports, the authors explain that vomiting is linked to so many different conditions that there’s no single test to figure it out. Instead, doctors have to rely heavily on clinical judgment—especially the patient’s medical history, symptoms, and physical exam—to decide what’s going on and how serious it is. “In the urgent care, in addition to asking about the symptoms themselves, I always ask questions about recent diet changes, places they may have eaten recently, ill contacts with similar symptoms, recent travel, camping or hiking around rivers or lakes, and any exposure to chemicals they may have had.”-MD name here
Mild causes of vomiting
Mild causes of vomiting include food-related issues, like overeating, food poisoning, a mild allergy, or an intolerance. The common stomach bug is also a mild issue that resolves on its own. Other mild causes can be a side effect from medication, or vomiting from pregnancy hormones.
Here’s a list of some of the most common and mild causes of vomiting:
- Diet-related issues
Eating too much, eating too fast, or consuming a lot of spicy or greasy foods can irritate the stomach and lead to nausea or vomiting. Mild food poisoning, caused by bacteria like Salmonella or E. coli, can also make you vomit within hours of eating the contaminated food. While uncomfortable, most cases resolve on their own with rest and hydration.
- Alcohol use
Drinking large amounts of alcohol in a short time can irritate the stomach lining, slow digestion, and trigger vomiting. Usually, this vomiting will resolve on its own, especially if you stop drinking. But if someone has been drinking very heavily and they can’t stop vomiting, they might have alcohol poisoning and will need medical attention to prevent dehydration.
- The stomach flu (viral gastroenteritis or norovirus)
Viral gastroenteritis is inflammation of the stomach and intestines caused by viruses such as norovirus, rotavirus, or adenovirus. It’s commonly called “the stomach bug” or “the stomach flu,” though it’s not related to influenza. In this case, the body triggers vomiting, and often diarrhea, to expel the virus from the system. Anyone who has had the stomach flu knows it can be very uncomfortable, but it typically resolves quickly, within a day or two.
Food poisoning and a stomach bug can be difficult to tell apart because they present with similar symptoms. Luckily, both are mild and usually resolve on their own.
- Motion sickness
People who are sensitive to motion, like car rides, boats, or planes, can develop nausea and vomiting when their inner ear and visual cues don’t match. It’s a common condition and usually improves once the motion stops. Over-the-counter remedies, such as Dramamine, can help alleviate symptoms.
- Medication side effects
Certain medications—like antibiotics, painkillers, antidepressants, and chemotherapy drugs—can upset the stomach and trigger vomiting. If a new medication is making you sick, it’s important to call your doctor. In most cases, the side effect is temporary and can be managed by adjusting the dosage or switching to a different medication.
- Pregnancy hormones (mild morning sickness)
In early pregnancy, rising hormone levels can lead to nausea and vomiting, which most people know as “morning sickness,” even though it can happen at any time of the day. While unpleasant, mild cases are common and usually fade by the second trimester.
- Cold or the flu
Viruses like the cold or flu can irritate the stomach lining and cause mild vomiting, especially in children. In most cases, it resolves on its own once the infection passes.
Moderately serious causes of vomiting
Moderate causes of vomiting are more serious than a simple stomach bug, but they don’t always require immediate emergency care. In many cases, conditions like vertigo, migraines, or heat exhaustion can improve with rest and home treatment. But if symptoms are severe, don’t go away, or keep coming back, it’s worth seeing a doctor to manage the issue and prevent it from happening again.
Here’s a list of some causes of vomiting that are moderately serious and should be monitored:
- Hyperemesis gravidarum
This is a severe form of morning sickness that causes persistent vomiting during pregnancy. If left untreated, it can require IV fluids and anti-nausea medication.
- Vertigo
Conditions like vestibular neuritis, Meniere’s disease, or benign paroxysmal positional vertigo (BPPV) can disrupt your balance system and trigger severe dizziness and vomiting. These are usually not emergencies, but they do require medical treatment to relieve symptoms and prevent falls.
- Heat exhaustion
You might vomit after extreme exercise, especially in the heat. It’s a warning sign that the body is overwhelmed. If symptoms are mild and improve with rest and fluids, you don’t need to go to the ER. If you suspect heat stroke, monitor the person closely because it could escalate to an emergency quickly.
Some high-risk individuals may experience heat exhaustion in extreme heat, even if they’re not exercising.
- Moderate food allergy or toxin exposure
Certain toxins (such as from spoiled food, mushrooms, shellfish, or meat) or mild food poisoning cases can cause ongoing vomiting without requiring ER-level care—unless the symptoms worsen or involve confusion, fever, or dehydration.
- Cannabinoid hyperemesis syndrome (CHS)
CHS is a condition where long-term, frequent cannabis use leads to repeated episodes of severe nausea and vomiting.
- Cyclic vomiting syndrome
Cyclic vomiting syndrome is a chronic condition that causes bouts of intense vomiting, up to four or more times per hour, for days. After a bout of vomiting, the patient usually remains symptom-free until the next flare-up. If episodes are frequent and long-lasting, they can lead to serious dehydration that requires specialist care.
Serious causes of vomiting
Serious causes of vomiting are life-threatening and require immediate medical attention. These include conditions like pancreatitis and appendicitis, blockages in the digestive tract, or dangerous conditions that trigger dangerous immune or neurological responses. Without urgent treatment, many of these conditions can worsen quickly.
When vomiting is related to a serious condition, it almost always comes with additional symptoms, like severe abdominal pain, confusion, high fever, chest pain, or other issues that come on suddenly and feel intense.
Here’s an overview of serious underlying conditions that can cause vomiting:
- Toxic ingestion
Swallowing toxic substances or overdosing on drugs will usually trigger vomiting. It requires urgent medical attention to prevent organ failure.
- Hepatitis from a virus, alcohol use, or medications
When the liver is overworked by toxins, such as alcohol, a virus, or certain medications, it can become inflamed, leading to hepatitis. This inflammation can trigger symptoms like nausea and vomiting. Vomiting may also be a sign that the liver is struggling to filter waste, particularly if it’s accompanied by fatigue, dark urine, or loss of appetite.
Moderate hepatitis (such as hepatitis A or early hepatitis B) usually doesn’t cause long-term damage in healthy people. But the situation becomes serious if you have chronic hepatitis B or C and develop jaundice, a sign that your liver may be starting to fail and needs urgent medical attention.
- Diabetic ketoacidosis (DKA) and gastroparesis
People with diabetes often develop gastroparesis, a condition where high blood sugar damages the nerve that controls how the stomach empties. This disruption can slow or stop digestion, leading to frequent nausea and vomiting. For people with diabetes, this means that it’s difficult to match food intake with insulin timing. These wide swings make blood sugar harder to control and can increase the risk of diabetic ketoacidosis (DKA). DKA is a life-threatening complication where the body produces too many acids called ketones in response to very high blood sugar. It causes rapid dehydration, vomiting, confusion, and deep, rapid breathing. Without quick treatment, DKA can lead to coma or even death.
- A blockage of the GI tract or the bowel
A bowel or GI tract blockage happens when something physically or functionally prevents food and fluids from moving through the intestines. Sometimes, there’s a physical block, such as scar tissue from surgery, a hernia, or a twisted section of the intestine. A twisted bowel can also cause sudden vomiting and bowel obstruction.
When this happens, digestion backs up, and you may start vomiting because the body can’t move contents forward. Without treatment, a blockage can lead to life-threatening complications like infection, tissue death, or bowel rupture.
- Anaphylaxis from a severe food allergy
This reaction may cause vomiting along with swelling, hives, and trouble breathing.
- Pancreatitis
Inflammation of the pancreas causes intense abdominal pain and vomiting.
- Appendicitis
Appendicitis is a condition when the appendix, a small organ in the GI tract, becomes inflamed and painful. Eventually, it can burst, causing sharp abdominal pain and requiring emergency surgery.
- Brain injury, tumor, or stroke:
A brain injury or tumor can cause increased intracranial pressure (ICP), which occurs when pressure builds up inside the skull due to trauma, a tumor, bleeding, or an infection. ICP can irritate the brain and trigger vomiting, often without nausea.
- Sepsis
Sepsis is a serious, body-wide infection that causes a range of symptoms, including vomiting, fever, and very low blood pressure.
- Heart attack
In some cases, a heart attack can cause nausea and vomiting, especially in women. Without quick treatment, a serious heart attack can lead to heart failure, permanent damage, or death.
- Severe bacterial infection (C. diff infection)
A Clostridium difficile (C. diff) infection primarily causes severe diarrhea, but vomiting occurs in serious cases. If someone with C. diff begins to vomit, especially if they have a high fever or signs of severe dehydration, they need urgent care.
- Cholecystitis
This condition is related to inflammation in the gallbladder. It comes with severe upper right abdominal pain, nausea, vomiting, and a fever.
- Crohn’s disease
Crohn’s disease is a lifelong, serious medical condition that has no cure, though its severity can vary from episode to episode. It can lead to complications such as intestinal blockages or bowel perforation. If a person with Crohn’s starts experiencing significant vomiting, it may be a sign of a serious episode.
- Ulcerative colitis
Ulcerative colitis is a chronic inflammatory bowel disease that affects the colon. Vomiting is not a common symptom, but it can occur during a severe flare-up. Vomiting in someone with ulcerative colitis should be taken seriously. t may signal a complication that needs urgent care.
- Colitis
Colitis is an inflammation of the colon. Usually, vomiting isn’t very common, but it can occur in severe cases.
- Kidney failure
In kidney failure, waste builds up in the blood because the kidneys can’t filter it out. This leads to uremia, a buildup of toxins in the body. If someone with weakened kidneys begins vomiting and experiencing fatigue, nausea, or confusion, it may signal a serious buildup of toxins and require emergency treatment, such as dialysis.
How can you treat mild vomiting at home?
To treat mild vomiting at home, it’s essential to begin rehydrating as soon as possible. Once you stop vomiting, begin introducing bland, small meals. You can also use over-the-counter antihistamines or anti-nausea medication, but this is usually not necessary. If your vomiting lasts longer than 48 hours or you develop severe symptoms, see a doctor.
Here’s an overview of what you can do to self-treat mild vomiting at home:|
- Rehydrate as soon as you can.
Once you can hold fluids, try drinking plenty of water, juice, or oral rehydration solutions (e.g., Pedialyte, or other water with electrolytes) as soon as possible. If you still feel nauseous or sick, try taking small sips. Be careful about drinking sports electrolyte drinks because they usually contain high levels of sugar that can make you feel ill, particularly on an empty stomach.
- Introduce bland foods (“BRAT” diet).
The “BRAT” diet stands for bananas, rice, applesauce, and toast. They represent a bland, low-fiber diet that is easy to digest. Experts recommend these and similar foods as you gradually transition back to normal eating.
- Try natural remedies.
Some doctors recommend eating ginger or peppermint to help settle your stomach. There’s only limited evidence to suggest these foods help, but if you’ve had good results in the past, they won’t do you any harm.
- Try OTC medications.
There are over-the-counter antiemetics, such as bismuth (the active ingredient in Pepto-Bismol) or dimenhydrinate (found in Dramamine), that can help reduce nausea and vomiting. However, for most mild cases caused by food or a stomach bug, clinical guidelines recommend allowing the illness to run its course. Taking medication may temporarily alleviate symptoms, but it doesn’t address the underlying cause.
Also, some of these drugs can cause side effects like drowsiness, constipation, or confusion, especially in older adults. That’s why experts generally suggest skipping medication unless the nausea is severe or clearly linked to something like post-op pain meds. If you’re still vomiting after 48 hours, it’s worth talking to a doctor.
How Doctor on Demand can assist with your vomiting
Doctor On Demand connects you with a board-certified physician in minutes, so you can get fast support for mild vomiting. Whether you need home care advice, a prescription, or want to talk through possible causes, you can get help from anywhere—no waiting room or appointment needed.
With Doctor On Demand’s virtual urgent care, you can get fast relief without leaving home. There’s no need to wait while feeling sick—just log in from any device with an internet connection, and a doctor will meet you where you are.
During your Doctor on Demand visit for vomiting, your physician will ask about your symptoms, medical history, and when the vomiting started. They’ll help you figure out possible causes, walk you through ways to feel better faster, and prescribe medications—like anti-nausea drugs—if needed, with pickup at your preferred pharmacy.
If your symptoms suggest something more serious, your doctor will explain the next steps and help you arrange any follow-up testing or in-person care.
How to prepare for your Doctor On Demand visit for vomiting
Before your virtual visit, please charge your device and find a quiet, well-lit spot with a reliable internet connection. Jot down when the vomiting began, any possible triggers, and other symptoms you’ve noticed. Write down any questions you have so you can get the most out of your visit.
Here’s a list of basic steps to take before your virtual Doctor on Demand visit for vomiting:
- Charge your device and check your setup.
It’s essential to ensure your phone, tablet, or computer is fully charged or plugged in. You can test your camera, microphone, and speakers in the Doctor on Demand platform ahead of time so you’re not scrambling to troubleshoot during the call.
- Pick a quiet, well-lit space.
If possible, sit in a private, well-lit area so your doctor can see you clearly and you can talk openly without interruptions.
- Note key information.
Jot down when the vomiting started, how often it’s happening, and anything you remember about what it looks like (e.g., color, whether it contains food particles). Also, jot down any other symptoms, like fever, abdominal pain, or dizziness. Also, include key information about any potential triggers like foods you’ve eaten, medication reactions, or potential exposure to the stomach flu. If you have any chronic conditions, like diabetes or GI conditions, be sure to mention them.
- Think about what you’d like to ask your doctor.
For example, you might wonder what you can do at home to manage the uncomfortable pain, or to regain strength. Or, you might ask whether you need medication or an in-person appointment.
- Keep your photo ID handy.
If your doctor prescribes medication, they may need you to verify your ID during the visit.
Doctor-answered FAQs for vomiting
Doctors answer common questions about vomiting, including when it’s worrisome, which red-flag symptoms to watch for, and how to prevent dehydration. You’ll also learn how to decide if you need in-person care, and what the ER can do to help.
How many times should I throw up before going to the ER?
There’s no exact number of vomiting episodes that means you need medical care. Experts say it’s more important to watch how long it lasts and how severe it gets. If you’re still vomiting after two days or can’t keep liquids down, go to the ER.
What do they give you in the ER to stop vomiting?
In the ER, doctors may give you anti-nausea medication like Zofran or Reglan, usually by IV. Not all vomiting patients will receive anti-nausea meds. The doctors make the call based on how severe your vomiting is, the likely cause, and your overall health history.
What is considered excessive vomiting?
There’s no strict clinical definition of excessive vomiting. But doctors generally consider it excessive if it happens frequently with little relief, like four times per hour for several hours, lasts more than 48 hours, or makes it impossible to keep down fluids.
Should I drink water after throwing up?
Yes, drink water if you can keep it down. Start with small sips. If water makes you vomit again, wait until you feel better before trying again. Staying hydrated is important, but if you can’t keep any fluids down for 12 hours or more, go to the ER.
What is considered uncontrollable vomiting?
Doctors may call vomiting “uncontrollable” if you can’t stop long enough to rest or keep fluids down. This usually means vomiting more than four times in an hour, for several hours in a row, or vomiting that continues for more than a day or two.
What color of vomit is worrying?
The most concerning colors are bright red and black. They mean there’s blood in your vomit and usually signal an upper GI bleed. Brown vomit can be a red flag, especially if you haven’t eaten anything brown or had a bowel movement in a while.
Should I go to the ER if my vomit is yellow?
Yellow vomit usually comes from bile and isn’t serious enough on its own to go to the ER, especially if you’re vomiting on an empty stomach. But if you also have severe abdominal pain, a fever, or signs of dehydration, go to the ER.
How much vomiting is too much?
How much vomiting is too much depends on your situation and health history. In general, vomiting for over two days, more than four times per hour for hours, or so often you can’t keep fluids down may signal something serious or cause dehydration. Seek care if that happens.
When to get IV fluids for vomiting?
If you go to the ER for vomiting, doctors will decide if you need IV fluids to replace lost water and electrolytes. Signs of severe dehydration include dark urine, dizziness, rapid heart rate, dry mouth, and low blood pressure.
What does the ER do for constant vomiting?
If you’re vomiting nonstop and can’t keep fluids down, ER doctors may give anti-nausea medication through an IV to help stabilize you. Then they’ll diagnose the underlying cause and begin appropriate treatment.
About the authors

Associate Medical Director, Specialty Care

Dr. Yvette Young is board-certified in Pediatrics and Pediatric Emergency Medicine with over twenty years of experience. She holds her medical degree from the University of Maryland and completed her residency and fellowship at Johns Hopkins, working at Level I trauma centers, including Children’s National Medical Center in Washington DC. In addition to her clinical work managing complex pediatric emergencies, Dr. Young has an MBA from Rutgers University, providing her with expertise in healthcare management, operations and strategic planning. She is a dedicated advocate for health equity and access to high-quality care for all children. Dr. Young lives in the Washington DC metro area with her family.



