Table of contentIn this article
- When to go to the ER for pink eye?
- When can you use telehealth for pink eye?
- When should you see an eye specialist for pink eye?
- When should you wait to see your primary care doctor for pink eye?
- What do hospital ERs do for your pink eye?
- Signs that your pink eye is serious
- What is commonly misdiagnosed as pink eye?
- High-risk groups for pink eye
- At-home treatments for mild cases of pink eye
- What are the different types of pink eye?
- How Doctor on Demand can assist with your pink eye right now
- Doctor-Answered Pink Eye FAQs
Pink eye can sometimes point to more serious eye problems. Find out when to go to the ER, when to call your doctor, and when home care may be enough.
When to go to the ER for pink eye?
Go to the ER if pink eye symptoms include severe eye pain, sudden vision changes, or light sensitivity. These may signal severe conditions that can damage your vision. Newborns with eye symptoms or anyone exposed to chemical irritants requires urgent care.
Head for your closest ER if you notice these symptoms:
- Intense eye pain, vision impairment, or light sensitivity (photophobia): Don’t wait if you’re dealing with intense eye pain, changes in vision, or discomfort in bright light. These symptoms may indicate severe eye conditions, such as corneal inflammation, intraocular swelling, or a sudden increase in eye pressure.
- You wear contacts, and your eyes turn red or pink. Stop wearing your lenses and see a healthcare provider right away if you experience redness in the white part of your eye (sclera). Contact lens users are at a higher risk of bacterial keratitis, especially infections caused by Pseudomonas aeruginosa, a bacterium that can rapidly damage the cornea. Prompt antibiotic treatment and medical assessment are critical.
- Newborns with pink eye symptoms: Babies under one month old with red eyes or discharge should be seen by a doctor without delay, as these signs may indicate serious infections acquired during birth. Causes of neonatal conjunctivitis include severe infections, such as those caused by Neisseria gonorrhoeae or Chlamydia trachomatis, bacteria commonly associated with sexually transmitted diseases. Without prompt treatment, these infections can cause severe complications, including blindness.
- Exposure to chemical irritants: If your eyes are exposed to chemicals such as acids or alkalis, rinse them thoroughly with clean water and seek emergency care immediately. Chemical injuries to the eye can cause permanent damage without rapid intervention.
- Persistent or worsening symptoms after treatment: If your eye irritation hasn’t cleared up after 7 to 14 days, or things are getting worse despite treatment, it’s time to follow up with a doctor. The cause might have been misidentified, the infection may be resistant, or another condition could be contributing to the issue.
- Follicular conjunctivitis: Viral infections, such as herpes simplex and adenovirus, or certain medications can cause this type of pink eye. It’s marked by small, raised bumps (follicles) on the inner eyelids and often causes redness, tearing, and mild discharge in one or both eyes.
- Severe or unusual discharge: Thick, pus-like discharge, especially if your eyelids stick together in the morning, may suggest a bacterial infection. Prevent complications with a medical evaluation and, if necessary, antibiotics..
- Keratoconjunctivitis: This more severe form of viral conjunctivitis affects both the conjunctiva and the cornea. When the cornea becomes involved, often in cases caused by adenovirus, symptoms like blurred vision, pain, and light sensitivity may develop. These signs should prompt medical evaluation, as they may require specialist care.
- Other symptoms in addition to pink eye: If you have pink eye along with symptoms such as a fever, cough, or skin rash, it may be part of a larger viral illness. Although it may not be urgent, having a doctor examine you can help identify the cause and guide you to proper care.
When can you use telehealth for pink eye?
You can use telehealth for pink eye if your symptoms are mild and your vision is fine. A doctor can often diagnose and treat it online, but you may still need an in-person visit for more severe symptoms.
In-person care is needed if you have severe pain, vision changes, light sensitivity, or if your child is very young. Contact lens wearers should be examined in person due to a higher risk of serious complications.
When should you see an eye specialist for pink eye?
See an eye specialist for pink eye if you have severe pain, vision changes, light sensitivity, symptoms that don’t improve, or wear contact lenses. Newborns and immunocompromised patients should also be evaluated promptly by a specialist.
See an eye specialist for pink eye if you or your child has:
- Severe eye discomfort, vision issues, or light sensitivity: See an eye doctor immediately if you’re experiencing sharp pain, trouble seeing clearly, or discomfort in bright light. These symptoms could signal severe conditions, such as inflammation inside the eye, corneal infections, or sudden pressure buildup.
- Pink eye symptoms in contact lens users: If your eyes become red or irritated while wearing contact lenses, remove them and consult an eye specialist. Contact lens wearers are more likely to develop rapidly progressing infections, such as bacterial keratitis, which can cause permanent eye damage if not treated promptly.
- Eye infections in newborns: Infants under one month old with swollen, red, or draining eyes should be examined by a doctor without delay. Newborn eye infections caused by bacteria, such as Neisseria gonorrhoeae or Chlamydia trachomatis, require immediate medical attention. They may lead to permanent vision damage if not treated promptly.
- Worsening or lingering symptoms: If eye irritation, discharge, or redness persists beyond 7 to 14 days or worsens despite treatment, it’s time to see a specialist. Ongoing symptoms may indicate a misdiagnosis, a resistant infection, or another condition that requires closer evaluation.
- Signs of corneal involvement: When pink eye is suspected to involve the cornea, as in cases of ulcers or keratitis, get a referral to an ophthalmologist right away. These symptoms can result in permanent vision loss or serious complications if left untreated.
- Conjunctivitis in immunocompromised people: People with weakened immune defenses are at higher risk for serious eye infections. If you’re immunocompromised and develop eye symptoms, see an eye specialist as soon as possible.
- Pink eye and COVID-19: In some cases, conjunctivitis may develop during a COVID-19 infection. Symptoms can include redness, tearing, a gritty feeling, and mild discharge. It often occurs in conjunction with a fever, tiredness, or a cough. COVID-19 related conjunctivitis is typically mild, and will likely resolve on it’s own, but if it persists beyond 7 days or is worsening over time, or there is eye pain, vision changes, or light sensitivity then evaluation is necessary.
When should you wait to see your primary care doctor for pink eye?
Wait to see your primary care doctor for pink eye if symptoms are mild, your vision is unchanged, and you haven’t had recent eye surgery, immune problems, or wear contacts. It’s also fine to wait if your child isn’t a newborn.
Most uncomplicated cases of pink eye, especially those involving mild viral or bacterial infections without vision changes or pain, can be safely treated by a primary care physician. A 2020 study in The Journal of Ophthalmic & Vision Research titled, “Conjunctivitis: A Systematic Review,” found that “approximately 1% of all patient visits to their primary care physician are conjunctivitis related.” It aded: “The first step in approaching a patient with presumed conjunctivitis is to rule out serious ocular conditions that present with ‘red eye,’ mimicking conjunctivitis.”
See your primary care doctor for pink eye in these situations:
- Mild symptoms without vision changes or severe pain: It’s usually safe to start with your regular doctor if your eyes are red, irritated, and producing watery or sticky discharge, but your vision is fine and you’re not in severe pain. These cases often improve with basic care.
- Not wearing contact lenses: If you don’t use contact lenses and have common pink eye symptoms, your primary care provider can typically manage your condition.
- No recent eye injury or surgery: Individuals without recent eye surgery or trauma who exhibit signs of conjunctivitis can typically initiate care with a primary care physician. A specialist should assess eye injuries or post-surgery symptoms right away.
- No immune system concerns: Most cases of uncomplicated conjunctivitis, especially viral or mild bacterial, can be managed safely by a primary care provider. Individuals with weakened immune systems are at a higher risk and may require the expertise of an ophthalmologist.
- Not a newborn: Babies under four weeks old with red or swollen eyes need urgent care to rule out severe infection. For older children and adults, mild cases are often safely treated with guidance from a primary care physician.
What do hospital ERs do for your pink eye?
In the ER, doctors check if a serious condition causes your pink eye. They may use special tools, do an eye exam, and give prescription drops if needed. If it’s more than pink eye, they’ll treat it right away.
Hospital emergency rooms may not be the best first choice for care, although people often turn to them as their initial point of contact. A 2017 research letter in the Journal of Ophthalmology, “Epidemiology of Conjunctivitis in US Emergency Departments,” reported that pink eye is the most common eye condition in hospital emergency departments, accounting for almost one-third of all eye-related emergency department visits. The researchers found that conjunctivitis cases in US emergency departments (EDs) peaked during early childhood, with a smaller peak in early adulthood, and that more cases presented in the spring. They recommended that educational efforts targeting new parents about conjunctivitis could divert young parents away from EDs, allowing patients requiring more urgent attention to receive better care.
If you do go to the ER, they will provide:
- Thorough evaluation of red or irritated eyes: Emergency doctors begin by asking detailed questions about symptoms, such as how long they’ve lasted, the type of discharge, and whether there is pain, blurred vision, or light sensitivity. They also check for the use of contact lenses. A slit-lamp exam helps detect corneal problems or foreign objects.
- Supportive care for viral pink eye: Most viral eye infections typically resolve on their own. ER treatment focuses on easing symptoms with cool compresses and lubricating drops. Patients receive guidance on how to prevent the disease from spreading. Antiviral medication may be prescribed if herpes simplex virus is suspected, especially if corneal involvement is present.
- Antibiotics for bacterial infections: While many bacterial infections resolve naturally, emergency doctors often prescribe antibiotics to speed recovery, especially for contact lens users, who are more likely to develop serious issues, such as corneal infections.
- Relief for allergy-related conjunctivitis: If allergies are the cause, treatment usually includes antihistamine or mast cell-stabilizing eye drops. Avoiding the allergen is also key. In more severe cases, short-term steroid drops may be used under medical supervision.
- Specialist referral when needed: ER providers refer patients to an ophthalmologist if they experience severe pain, vision changes, light sensitivity, contact lens-related infections, or suspected bacterial infections from gonorrhea or chlamydia, or if symptoms fail to improve despite treatment.
- Infection prevention protocols: Hospitals use strict safety measures to prevent the spread of infectious conjunctivitis, also known as pink eye. Protocols include handwashing, wearing protective gear, and isolating contagious patients when necessary.
Signs that your pink eye is serious
Pink eye is considered serious when it causes eye pain, vision changes, light sensitivity, or symptoms that worsen or don’t improve. People who wear contact lenses, have weak immune systems, or develop thick discharge should seek medical care right away.
See a doctor right away if you notice any of the following signs. They may point to conditions that can threaten your sight if not treated quickly:
- Eye pain: Typical pink eye may feel scratchy or irritating, but it shouldn’t cause real pain. If your eye starts to hurt — especially if the pain is sharp, deep, or getting worse — it could mean there’s inflammation or infection deeper in the eye. Conditions such as keratitis, uveitis, scleritis, or endophthalmitis all require urgent medical attention and can lead to vision loss if left untreated.
- Blurry vision: Most cases of pink eye don’t blur your vision. If your sight becomes hazy or you’re having trouble focusing, that’s a warning sign. Blurred vision could mean the cornea is involved, or that inflammation is affecting internal parts of the eye, not just the surface.
- Light sensitivity: If your eyes are suddenly sensitive to light, so much so that you find it painful to be outside or look at screens, you might be dealing with more than conjunctivitis. Light sensitivity, or photophobia, is often a sign of conditions like keratitis or uveitis, which need evaluation by an eye specialist.
- Severe or spreading redness: Redness is part of almost every case of pink eye, but extreme or worsening redness may be a sign of a more serious problem. Widespread redness, especially if it looks deeper or is accompanied by swelling, could point to internal inflammation or a more aggressive infection.
- Thick yellow-green discharge: Bacterial conjunctivitis can cause discharge, but if it’s thick, yellow-green, and builds quickly, that could mean something more dangerous, such as gonococcal conjunctivitis, a fast-moving infection that requires immediate treatment to prevent damage to the eye.
- Contact lens use: Wearing contacts increases the risk of corneal infections like bacterial keratitis, which can look like pink eye at first but turn serious fast. If you wear contacts and develop red, irritated eyes, take your lenses out right away and call an eye doctor.
- Recent eye injury or surgery: If your eye has been injured or you’ve had surgery recently, don’t assume it’s just pink eye. Post-operative or trauma-related redness could signal endophthalmitis, a serious infection inside the eye. This is a medical emergency and needs to be evaluated immediately by an ophthalmologist.
- Weak immunity: If you’re immunocompromised, because of a chronic illness or medications that suppress your immune system, you’re at higher risk for severe or unusual eye infections. Even mild-looking pink eye symptoms in these cases should be checked out promptly by a medical professional.
What is commonly misdiagnosed as pink eye?
Red or irritated eyes don’t always mean you have pink eye. In fact, many other conditions can cause similar symptoms, making it easy to misdiagnose, especially in the early stages. These conditions include allergies, blepharitis, a scratched cornea, and more. A misdiagnosis can delay proper treatment.
These are some of the most common look-alike conditions that can be mistaken for conjunctivitis:
- Allergy-related eye irritation: Allergies often trigger itchy, watery, and red eyes—symptoms that overlap with viral conjunctivitis. But allergic reactions usually affect both eyes at the same time and often come with sneezing or nasal congestion. Unlike infections, allergic flare-ups aren’t contagious and often respond to antihistamines or allergy drops.
- Eyelid inflammation (blepharitis): This is an inflammation along the lash line, not the surface of the eye itself. It causes crusting, redness, and irritation, especially when you wake up. Patients sometimes assume it’s pink eye, but the focus of the irritation is the lids. Gentle cleansing and warm compresses are the first step. In more stubborn cases, doctors may prescribe antibiotic or steroid drops.
- Blepharoconjunctivitis: This condition involves both the eyelids and the conjunctiva. It tends to be more persistent than basic pink eye and often shows up with greasy, crusted lashes and chronic irritation. It’s frequently linked to skin conditions like rosacea and usually needs long-term care, not a one-time prescription.
- Blocked tear ducts: In infants, extra tearing and discharge can look a lot like pink eye. But if the tear duct is blocked, tears can’t drain properly, and bacteria can build up. Many cases resolve without treatment, but persistent symptoms should be checked by a pediatrician or eye doctor.
- Scratched cornea (corneal abrasion): A corneal scratch can cause redness, tearing, pain, and light sensitivity—all things people associate with pink eye. But the key difference is that corneal abrasions usually follow an injury or contact lens mishap. These need quick attention to prevent infection and support healing.
- Chronic dry eyes: Dryness may not sound serious, but it can cause redness, burning, and even blurred vision. Unlike conjunctivitis, dry eye usually gets worse throughout the day and isn’t contagious. It’s more common in older adults, screen-heavy lifestyles, or dry climates. Lubricating drops help, but long-term relief may require more than just over-the-counter solutions.
- Episcleritis and scleritis: These are inflammatory eye conditions that affect deeper layers beneath the conjunctiva. Episcleritis is generally mild and causes a patch of redness without much discomfort. Scleritis, on the other hand, is painful and can threaten vision. Either one might initially look like pink eye, but they require a different diagnostic approach and more specialized treatment.
- Foreign matter in the eye: Dust, sand, or even an eyelash can irritate the eye enough to cause redness and tearing. If something stays lodged under the lid or scratches the eye’s surface, the symptoms can be mistaken for conjunctivitis. If flushing the eye doesn’t help, it’s best to have a doctor examine it.
- Corneal infection (keratitis): Keratitis is far more serious than pink eye, but early symptoms like redness and tearing can overlap. The big red flags are pain, blurred vision, and sensitivity to light, especially in contact lens users. This condition requires prompt medical care to prevent permanent corneal damage.
- Stye (hordeolum): A stye is a small, painful bump along the eyelid, often filled with pus. It can cause local redness and tenderness, which some people assume is pink eye. But unlike conjunctivitis, the irritation is confined to one spot. Warm compresses are usually enough, though antibiotics may be needed in some cases.
- Broken blood vessel (subconjunctival hemorrhage): A bright red patch on the white of the eye can look alarming and like a possible infection. But it’s usually painless, doesn’t affect vision, and clears up on its own within a week or two. No treatment is needed unless it recurs frequently.
- Thyroid-related eye problems (Graves’ disease): In autoimmune thyroid disease, the eyes can become red, watery, or gritty. It’s easy to confuse this with conjunctivitis. But Graves’ eye disease typically involves bulging eyes, eyelid retraction, or trouble moving the eyes. Blood tests and imaging help confirm the diagnosis.
- Inflammation inside the eye (uveitis or iritis): These are internal eye inflammations that sometimes masquerade as pink eye early on. The difference is that uveitis often comes with light sensitivity, deeper aching pain, and blurred vision. Left untreated, it can cause permanent damage, so it needs steroids or immunosuppressive treatment under the care of a specialist.
High-risk groups for pink eye
While anyone can get pink eye (or conjunctivitis), some are definitely more prone to it.
- Children: We often see it more frequently in children, especially those in daycare or school, as germs spread easily in these environments.
- Immunocompromised: People with weakened immune systems or conditions like diabetes are also more susceptible.
- Contact lens wearers: Being extremely careful with cleaning is key; otherwise, they’re at a higher risk.
- Allergy sufferers: If you suffer from seasonal allergies, you’re more likely to get pink eye, as you tend to rub your eyes more due to irritating allergens.
- Poor hygiene: Those who aren’t great about washing their hands regularly or tend to share personal items like towels or makeup can easily spread it to themselves.
- Contact with someone who has conjunctivitis: if you’ve been in close contact with someone who already has conjunctivitis, like a family member or roommate, your risk goes up.
- Having viral conjunctivitis: If you’ve recently had a cold or the flu, pink eye (viral conjunctivitis) can sometimes tag along with those viral infections.
At-home treatments for mild cases of pink eye
There are many ways you can take care of your pink eye at home. First off, it’s good to know that lots of pink eye cases—or “conjunctivitis” as we call it—can actually get better right in your own home.
So, here’s what you can do:
Warm or cool compresses: You can use either. Whatever feels best for your eyes. Just grab a clean cloth, soak it in warm or cool water, and gently place it over your closed eyes. This can really help with the discomfort.
Lubricating eye drops: You know, those “artificial tears”? You can pick these up over the counter at any pharmacy. They’re great for soothing that dry, gritty feeling that often comes with pink eye.
For itchy, irritated eyes (especially with viral infections or allergies): If your eyes are super itchy or irritated, an over-the-counter eye drop with an antihistamine or decongestant can be really helpful. Just make sure it’s a “topical ophthalmic” one, meaning it’s meant for your eyes. This is particularly good if we suspect it’s a viral pink eye or an allergic reaction.
Now, here’s something that often surprises people. Dr. Eirich, from Included Health, states, “Even if your pink eye is caused by bacteria, these same home treatments can really help. It might sound strange, but studies actually show that most bacterial pink eye cases will clear up on their own without needing an antibiotic. So, don’t be surprised if we don’t jump straight to antibiotics. We often start with these comforting home remedies first, and for most people, that’s all they need to get better.”
What are the different types of pink eye?
Not all pink eye is the same. The irritation can come from infections, allergic reactions, or even chemical exposure, and how it’s treated depends on what’s behind it. Here’s how to recognize the main types and what separates them.
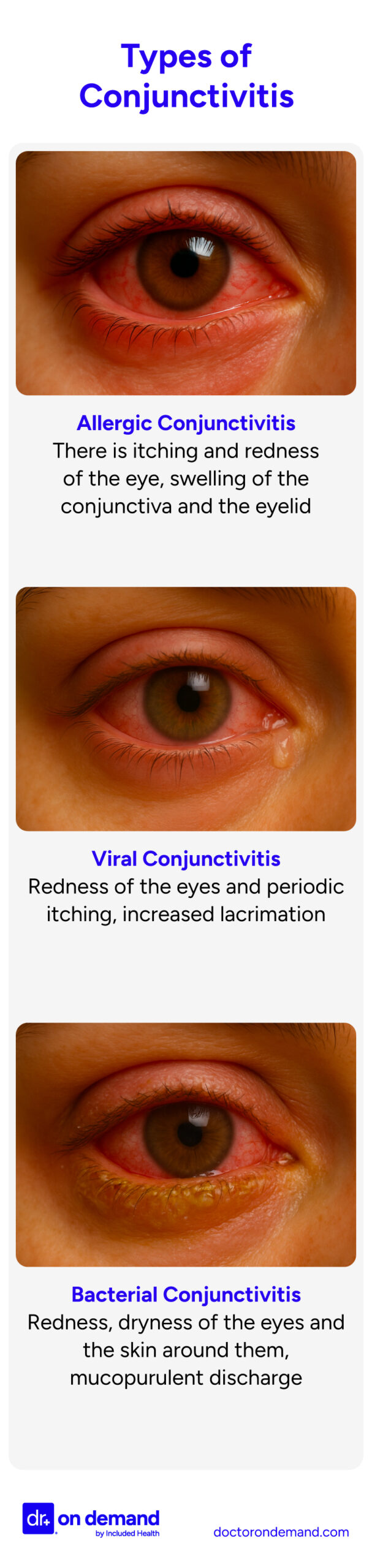
Allergic conjunctivitis
This type tends to show up during allergy season or after being around pets, dust, or mold. Both eyes are usually involved, and the itch can be intense. You might also notice tearing, swelling, or a mild burning feeling. If you’re also sneezing or congested, it’s probably tied to allergies rather than infection. Since there’s no virus or bacteria involved, it isn’t contagious. Relief often comes from cool compresses, over-the-counter allergy drops, and avoiding whatever triggered the reaction. If symptoms don’t improve, doctors may suggest a short course of stronger medication.
Bacterial conjunctivitis
This kind of pink eye comes from bacteria, not a virus or allergy. It often starts in one eye, causing it to turn red, feel irritated, and produce thick discharge. You might notice your eyelid sticking shut in the morning. The second eye may start to bother you a little later. Doctors frequently prescribe antibiotic drops or ointment to clear it faster, though mild cases sometimes go away on their own. If you wear contacts, stop using them for now and check in with an eye care provider. Infections like these can escalate quickly in contact lens users if not treated early.
A 2023 review from the National Institutes of Health described bacterial conjunctivitis as less common than viral or allergic types, but often more complex to manage, especially when diagnosis is delayed.
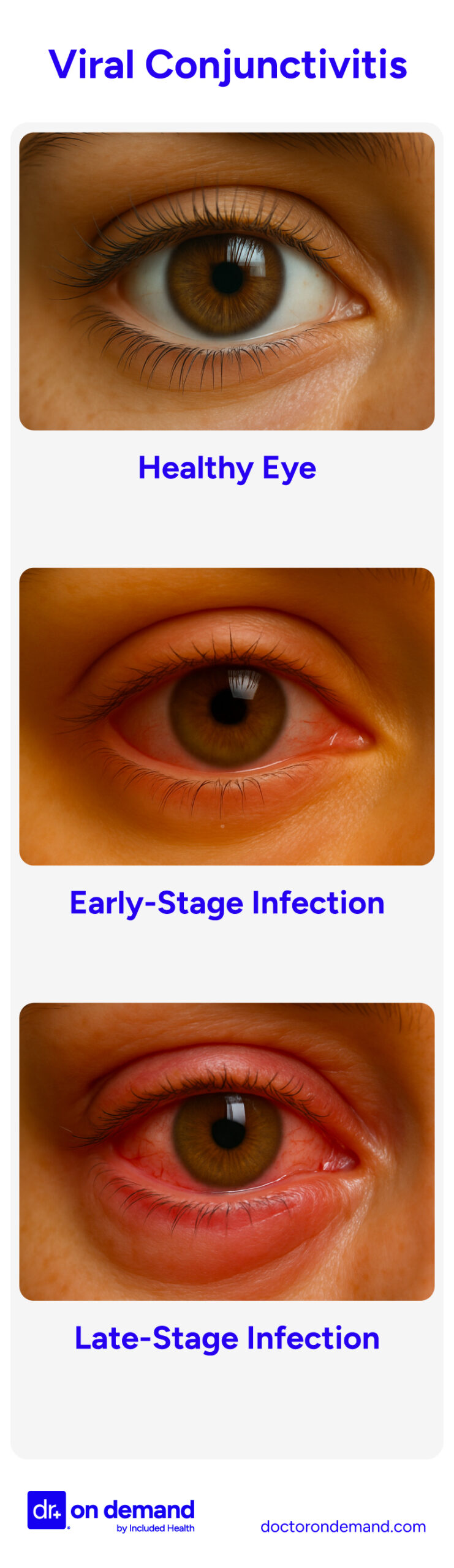
Viral conjunctivitis
This is the version most people run into, especially during cold and flu season. It usually hits one eye first, then moves to the other. The discharge is watery or mucoid, not thick, and your eye may sting or feel like something’s in it. Sometimes there’s swelling near the front of your ear. There’s no instant fix, but most people feel better in a week or so. Herpes simplex virus can also cause viral conjunctivitis, though it’s less common. Herpes eye infections are typically more painful than other viral or bacterial conjunctivitis. These cases require antiviral treatment and often specialist follow-up. In the meantime, good hygiene is your best defense against spreading it to others.
A more severe subtype, known as epidemic keratoconjunctivitis (EKC), involves both the conjunctiva and the cornea. It’s caused by certain strains of adenovirus and can lead to light sensitivity, blurred vision, and prolonged symptoms. When the cornea is involved, follow-up with an eye specialist is often recommended.
Chemical conjunctivitis
This form doesn’t involve germs. It’s triggered by exposure to substances that irritate the eye—anything from pool chlorine to strong household cleaners. Eyes may burn, turn red, and start tearing almost immediately. If the substance is particularly harsh, like an industrial cleaner or strong acid, the eye can sustain damage. Flush the eye with lots of clean water right away. After rinsing, the right treatment depends on what got in and how the eye responds over the next few hours. Some people bounce back quickly, while others may need closer follow-up.
Giant papillary conjunctivitis
This type develops over time and is usually linked to long-term contact lens use. It’s not caused by infection. Instead, the inner part of the upper eyelid becomes inflamed and forms small bumps that rub against the eye. This can lead to discomfort, blurry vision, and more mucus than usual. Lenses might feel scratchy or start moving around more than they used to. Taking a break from lens wear usually helps. Switching to a different lens type or using prescription eye drops may also make a difference.
Neonatal conjunctivitis
When a newborn develops red, swollen eyes and discharge within the first couple of weeks after birth, it could be neonatal conjunctivitis. This condition can come from bacteria or viruses the baby was exposed to during delivery. Infections linked to gonorrhea or chlamydia can turn serious quickly, which is why doctors often treat right away—sometimes with IV antibiotics if needed. Hospitals routinely apply protective eye ointment to newborns just after birth, not because there’s a known problem, but as a precaution against infections that can develop before any symptoms appear.
How Doctor on Demand can assist with your pink eye right now
Doctor On Demand assists patients by providing a convenient option for diagnosing and treating pink eye through online visits. Whether your eye condition is mild or acute, find 24/7/365 virtual care for fast answers and treatment options without leaving home.
Many conditions mimic pink eye, and your Doctor on Demand provider can help you distinguish between them. Telehealth urgent care providers can diagnose and treat your eye condition, as well as prescribe medications, including antibiotics, if needed.
Skip the wait at a clinic and get expert care for pink eye with a virtual urgent care appointment today.
How to prepare for your Doctor on Demand visit for pink eye
If you’re experiencing symptoms of pink eye (conjunctivitis) and have scheduled a virtual consultation through Doctor On Demand, proper preparation can enhance the effectiveness of your visit. By preparing your technology, medical information, and environment, you can maximize the benefits of your Doctor On Demand telehealth visit for pink eye.
A few simple steps can make your virtual visit go more smoothly and help your provider assess your eye problem accurately:
- Check your setup: Use a charged phone, tablet, or computer with a working camera and microphone. Find a spot with strong Wi-Fi and good lighting so the doctor can see your eyes clearly.
- Gather your info: Write down when your symptoms started, how they’ve changed, and anything that makes them better or worse. Also note any recent illnesses, allergies, or past eye issues.
- List your medications: Be ready to share any prescriptions, over-the-counter remedies, or eye drops you’ve used.
- Pick a quiet place: Choose a well-lit, private space where you can speak freely and avoid distractions during the appointment.
While many cases of pink eye can be handled through telehealth, some symptoms call for in-person care. If your provider suspects something more serious, they’ll explain what to do next, including when and where to follow up.
Doctor-Answered Pink Eye FAQs
Here are frequently asked questions regarding how you get pink eye, how to identify it, how long the condition lasts, and effective treatments.
When will pink eye go away on its own?
Viral pink eye usually clears within 7 to 10 days without treatment. Bacterial types often resolve in 2 to 5 days, though symptoms can last longer. Allergic conjunctivitis improves once the allergen is removed. See a doctor if symptoms worsen or persist beyond two weeks.
How do you know when you get pink eye?
Pink eye often causes redness, tearing, discharge, and irritation in one or both eyes. You might feel as if something’s in your eye, and your lashes may stick together in the morning. If you have pain or vision changes, get checked by a medical professional.
What do you do for a newborn who has pink eye?
If a newborn has red or swollen eyes, discharge, or crusted lashes, contact a doctor right away. Newborn eye infections can become serious quickly and require urgent treatment to protect vision. Never attempt home treatment before getting medical guidance.
When should a child be taken to the doctor for pink eye?
See a doctor if your child has eye pain, swelling, yellow or green discharge, vision problems, or symptoms that don’t improve within a few days. Prompt care is also important if both eyes are affected, or your child has a fever or wears contact lenses.
How long should you wait before getting medical care for pink eye?
If symptoms don’t improve within three to five days, or if there’s eye pain, swelling, or vision changes, seek medical care. Newborns, contact lens users, and people with weakened immune systems should be evaluated promptly, even for mild symptoms.
How do you know you are completely over pink eye?
You’re likely recovered when redness, swelling, and discharge are gone, your eyes feel normal, and vision is clear. Crusting should stop, and your eye should no longer feel gritty. If symptoms return after treatment, follow up with your healthcare provider.
When is pink eye contagious?
Viral and bacterial pink eye are contagious while symptoms like tearing and discharge are present. Bacterial infections are usually no longer contagious 24 hours after starting antibiotic drops. Viral pink eye may remain contagious until all symptoms resolve.
When does pink eye stop being contagious?
Pink eye is typically no longer contagious once the eye is clear, symptoms are gone, and any discharge has stopped. For bacterial cases, that’s usually 24 hours after starting antibiotics. Viral infections often remain contagious until the eye looks and feels completely normal.
How long does it take for pink eye to go away?
Most cases resolve within one to two weeks, depending on the cause. Viral pink eye lasts about a week, bacterial types often improve within days of treatment, and allergic conjunctivitis improves once the trigger is removed. See a doctor if symptoms worsen or linger.
When should you return to a doctor for pink eye symptoms?
Return to your doctor if symptoms worsen or fail to improve after three to five days of treatment. Red flags include pain, blurry vision, thick discharge, or swelling. Babies and people with weakened immunity should be seen again if any symptoms persist or recur.
About the authors

Board-certified in emergency medicine, Dr. Melissa Eirich brings over three decades of clinical experience to her practice. Prior to joining Doctor On Demand in 2019, Dr. Eirich dedicated over ten years as an associate professor of clinical emergency medicine at the University of Rochester in New York and also worked in urgent care settings. In addition to her clinical practice, Dr. Eirich maintains a significant focus on medical education at Included Health.

Quan Lam is a copywriter with over 15 years of experience writing and editing content for both start-ups and legacy brands, as well as 2 years of writing experience exclusively within the healthcare space. She currently lives and works in New York City.



