Table of contentIn this article
- When to take your child to the ER for the flu
- Common flu symptoms in children
- Serious flu symptoms in children
- How to identify when your child has the flu
- Timeline of flu symptoms in children
- What will the hospital ER do if your child has the flu
- Common complications of the flu for children
- How Doctor on Demand can assist your child with the flu
- Doctor-answered children’s flu FAQs
While most flu cases in children are mild, some can turn serious fast. This guide will help you recognize when symptoms may signal a medical emergency, — and explains when to go to the ER, call your doctor, use telehealth, or, for mild cases, treat your child at home.
When to take your child to the ER for the flu
If your child exhibits serious flu symptoms, you should take them to the ER for evaluation. Serious symptoms include respiratory distress (often accompanied by bluish lips or skin), unresponsiveness or confusion, chest pain, seizures, severe dehydration, persistent high fever, or worsening symptoms after initial improvement.
These signs may indicate that your child is at risk for more serious complications, such as pneumonia or encephalopathy. Flu symptoms can escalate quickly, even in otherwise healthy children. That’s why it’s important to act quickly if your child is under 2 years old or has a weakened immune system.
In a 2021 review in the journal Children titled “Hospitalization of Children Aged <5 Years Due to Influenza: Study Based on the National Hospitalization Registry,” the authors write, “Influenza viruses can cause severe illness and complications in children, including pneumonia, myocarditis, and neurologic complications such as encephalopathy or seizures.”
ERs are well-equipped to perform advanced testing and provide supportive care, such as IV fluids or oxygen, if needed. Trust your instincts. If your child is exhibiting serious symptoms, do not hesitate to seek care.
“Parents know their child best. If something feels off — especially if your child is breathing fast, unusually sleepy, or not drinking — it’s always safer to get checked.” – Brian Knox, MD
When to call 911 when your child has the flu
Call 911 if your child has severe flu symptoms that require immediate medical care. This includes life-threatening signs such as seizures, difficulty breathing, bluish lips or skin, or unresponsiveness. In these situations, it’s safer to call for emergency help than to drive to the hospital yourself.
Paramedics can begin treatment right away like — providing oxygen, managing seizures, or supporting breathing — as they transport your child. That early intervention can save precious time and lead to better outcomes.
When you can use telehealth for your child’s flu
There are no formal guidelines, but generally, telehealth is appropriate for a child with less serious symptoms and who is otherwise well-hydrated, responsive, exhibits stable behavior, and has no breathing issues. They can receive remote diagnosis and treatment, including initial antiviral intervention.
A telehealth visit for the flu will help to determine if any of your child’s symptoms require further evaluation or if they need testing to determine whether they have a common flu or perhaps a more serious illness, such as RSV or COVID-19.
The provider will recommend in-person care with your pediatrician or at the hospital if your child has serious symptoms such as a persistent high fever over 104°F, signs of dehydration, or trouble breathing, or if any concerns arise during the telehealth visit.
When to call your pediatrician for your child’s flu
Call your pediatrician for further guidance if your child’s flu symptoms include a fever lasting more than 3-5 days, inadequate fluid intake, urinating less than every 8 hours, or lethargy and other symptoms that are concerning but are not severe enough for an emergency room visit.
Your pediatrician knows your child’s health history and will help determine if your child’s symptoms are common to a seasonal flu or indicative of a more serious illness. A pediatric visit may include a physical examination, flu testing, and guidance on any necessary further medical intervention. Your pediatrician may also be able to rule out other underlying illnesses such as strep throat, ear infections, or COVID-19.
Knowing what to do when your child has the flu can feel overwhelming, but exploring flu remedies that can ease symptoms may help you feel more confident about how to care for them and when to seek additional help.
Common flu symptoms in children
Recognizing the signs of flu in children can help you decide when to monitor at home and when to seek medical help. While not every child will exhibit the same symptoms, a combination of key indicators often suggests influenza.
Pay attention to both the onset and progression of symptoms. Noting this timeline will help your child’s doctor assess the situation more effectively.
Here are some of the most common flu symptoms in children:
- Fever above 100.4°F (38°C): For babies under 3 months, any fever of 100.4°F or higher needs immediate medical attention, as it could signal a serious infection. In toddlers and older children, a temperature above 102.2°F is considered high and should be watched carefully. Track how long the fever lasts and whether it responds to medication.
- Cough: Flu-related coughs may be dry or phlegmy and tend to linger longer than other symptoms. If your child’s cough worsens or starts interfering with eating or sleeping, it’s a good idea to call your pediatrician.
- Sore throat: A sore throat is often one of the early signs of the flu. If it becomes severe enough to prevent your child from eating or drinking, seek medical advice.
- Runny nose: Congestion and nasal discharge are common. While clear mucus is typical early on, it may turn yellow or green during recovery. That’s not always a cause for concern — but if the discharge worsens or sticks around for more than 10 days, it could point to a secondary infection.
- Headache: Headaches can be part of the flu’s symptom profile. If your child also develops neck stiffness or sensitivity to light, call your doctor, as these signs could signal something more serious.
- Body aches: Muscle and joint pain are common during the first few days of flu and can make kids feel especially run down. As long as the pain doesn’t intensify or become severe, it’s usually part of the normal course of illness.
- Fatigue: Tiredness often appears early and may last several days. If your child seems too drained to eat, drink, or stay engaged, that could be a sign the flu is taking a more serious toll and warrants medical attention.
- Abdominal pain: Some children with the flu may complain of stomach pain, especially early in the illness. It’s often mild and may occur alongside nausea, vomiting, or fever. However, if the pain is severe, persistent, or localized, a doctor should evaluate it.
Serious flu symptoms in children
There are times when flu symptoms are more serious and require more immediate attention. These symptoms may indicate complications or more serious illnesses such as pneumonia, dehydration, or neurological issues. Knowing what to look for can help you act fast and get the care your child needs.
Serious flu symptoms include:
- Difficulty breathing: If your child is struggling to breathe, exhibits fast or labored breathing, flared nostrils, or chest retractions (sucking in between the ribs), they may be in respiratory distress.
- Bluish lips or skin: The presence of bluish lips or skin can indicate low oxygen levels and the need for emergency care. Pay close attention to the lips, fingertips, and facial areas.
- Altered mental status: If your child is hard to wake, disoriented, or extremely irritable, it may be a sign of a more severe illness or neurological issue. Seek care immediately.
- Chest pain: Complaints of chest pain, particularly if accompanied by difficulty breathing or worsened by activity, should be taken seriously, as they may indicate pneumonia or heart-related issues.
- Seizures: Seizures associated with the flu may be caused by high fever or more serious brain inflammation and should be evaluated at an emergency room as soon as possible.
- Inability or refusal to walk or move: If a child refuses to stand, walk, or move their limbs, it may be a sign of severe muscle pain or inflammation, weakness, or overall pain associated with the flu.
- Severe dehydration: This can include a dry mouth, minimal urination, or sunken eyes or fontanelle. All indicate your child is not getting enough fluids due to fever, vomiting, diarrhea, or refusal or inability to drink liquids. If your child has not had any fluids for an extended period or has not urinated in over 8 hours, they require IV fluids to rehydrate.
- High, persistent fever (especially over 104°F): A fever that remains high despite appropriate doses of fever-reducing medication may indicate a worsening infection or complication. While fevers over 104°F are not uncommon with the flu, persistent or unresponsive high fever should be evaluated by a healthcare provider.
- Dizziness or lightheadedness: Feeling faint, unsteady, or dizzy may be a sign of dehydration, low oxygen levels, or worsening illness. If your child has trouble standing, complains of the room spinning, or seems unusually unsteady, seek medical attention.
- Rash with flu symptoms: A rash isn’t typical with flu, but if your child develops one — especially alongside high fever, irritability, or other concerning signs — it could signal a secondary infection or more serious condition and should be evaluated promptly.
- Return of symptoms after initial improvement: If your child starts to recover but then develops new or worsening symptoms — such as fever, cough, or fatigue — this may signal a secondary bacterial infection like pneumonia or sinusitis and should be evaluated by a doctor.
Non-serious flu symptoms in children
The flu is a common illness in children of all ages, and many symptoms are non-serious and will resolve on their own with time and rest. Less serious flu symptoms include mild fever, sore throat, cough, runny nose, headache, body aches, chills, and fatigue. These symptoms, absent any more serious concerns, are uncomfortable but usually improve within a week of onset.
You know your child better than anyone, but generally speaking, if your child is alert and breathing well, follow these five simple steps for early treatment of the flu or common cold.
How to identify when your child has the flu
Identifying the flu in your child involves monitoring symptoms and using rapid testing to distinguish it from more serious illnesses, such as RSV (respiratory syncytial virus) or COVID-19, both of which can have similar symptoms.
Recognizing the flu in children begins with noticing how quickly symptoms appear and what they are. Unlike the common cold, the flu typically develops suddenly. A child who seemed fine in the morning may develop a high fever, body aches, chills, or fatigue by the afternoon. A dry or persistent cough, sore throat, or runny nose often accompanies these early signs. Some children also experience headaches or symptoms like nausea or mild vomiting, especially early in the illness.
The flu shares symptoms with other respiratory illnesses, including COVID-19 and RSV, making it challenging to distinguish between them based solely on symptoms. That’s why it’s important to pay particular attention to the severity and timing of your child’s symptoms. The flu is known for its abrupt onset and pronounced fatigue and muscle aches. If your child’s symptoms are intense and began quickly, the flu is a likely suspect.
In a 2023 study in Clinical Infectious Diseases titled “The Spectrum of Influenza in Children,” the authors note that children “are far less likely to be asymptomatic with influenza than adults, and asymptomatic young children are still very likely to shed virus.” That means that even children who do not seem to be sick but are infected with influenza are likely to be contagious.
Rapid flu testing can help confirm the diagnosis. These tests are most accurate when performed within the first 48 hours after symptoms begin, which is also the optimal window for antiviral medications. In many cases, a test may not be necessary if the symptoms clearly match the flu and the child is otherwise healthy. Testing becomes more important if your child is at higher risk or shows signs of complications.
Ultimately, knowing what to watch out for and when to seek help can make a big difference. If symptoms appear suddenly and match the typical flu profile, keep your child home from daycare, monitor for worsening signs, and contact your pediatrician if you’re unsure.
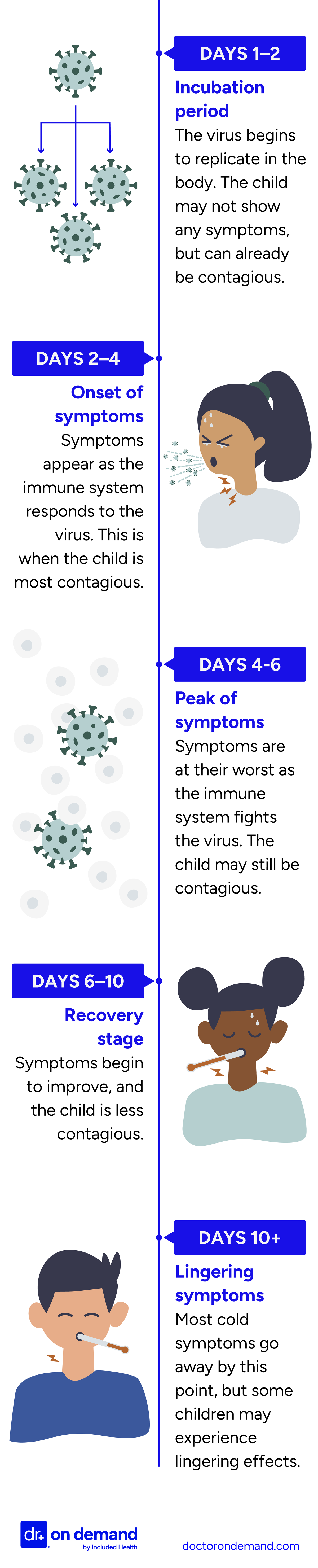
Timeline of flu symptoms in children
Flu vs. common cold vs. RSV vs. COVID-19
| Symptom | Flu | Common Cold | RSV | COVID-19 |
| Onset of Symptoms | Abrupt | Gradual | Gradual | Varies |
| Fever | High (over 104°F) | Low-grade or none | Low to moderate | Varies |
| Congestion | Common | Very common | Common | Common |
| Cough | Dry or productive | Mild | Wet-sounding | Dry or Productive |
| Body Aches/Fatigue | Prominent | Mild or absent | Uncommon | Sometimes |
| Breathing Issues | In severe cases | Rare | Common in infants | Possible |
| Wheezing | Rare | No | Common in infants | Rare |
| Loss of Taste/Smell | Rare | Rare | No | Common in older children and teens |
| Seasonality | Fall-Winter | Year-round | Fall-Winter | Year-round |
| Age Group | All ages | All ages | Severe in infants | All ages |
Regular flu vs Influenza A vs Influenza B in children
Mild cases of seasonal flu caused by influenza A or B typically look the same in children, and symptoms alone won’t distinguish between them. However, influenza A tends to cause larger outbreaks and often peaks earlier in the season, while influenza B may peak later. Testing is the only way to tell the difference, but treatment and monitoring are the same for both.
| Symptom | Regular/seasonal flu | Influenza A | Influenza B |
| Fever | Yes | Common-High | Common-High |
| Cough | Yes | Common | Common |
| Fatigue/body aches | Yes | Often pronounced | Often pronounced |
| Onset | Sudden | Sudden | Sudden |
| Vomiting/diarrhea | Sometimes | Possible (more common in children) | Sometimes |
| Seasonal pattern | Varies | Peaks | Peaks later in the season |
| Severity | Varies | Can be severe | Usually less severe |
| Pandemic potential | No | Yes | No |
| Testing needed to distinguish? | Yes | Yes | Yes |
| Age group | All ages | More severe in children | All ages |
What will the hospital ER do if your child has the flu
If your child is taken to the ER for the flu, the care team’s priority is to identify any complications and start appropriate treatment right away. The visit typically includes a physical exam, vital signs check, testing, and supportive care based on the severity of your child’s symptoms.
Here’s how the ER visit usually unfolds:
- Triage and initial assessment
When you arrive, a nurse or clinician will check your child’s vital signs, including temperature, heart rate, breathing rate, oxygen levels, and blood pressure. These measurements help the team decide how urgent the situation is. If your child has fast breathing or low oxygen saturation, they’ll be seen right away, as these may point to complications like pneumonia or dehydration. - Medical exam and diagnostic testing
A doctor will examine your child and ask about their symptoms, when they began, and how they’ve changed. Depending on the situation, they may order a rapid flu test or a respiratory panel that also checks for COVID-19 and RSV. If there’s concern about pneumonia, dehydration, or a bacterial infection, your child might also need a chest X-ray or blood tests. - Antiviral medication
If the flu is confirmed or strongly suspected, your child may be given an antiviral like oseltamivir (Tamiflu). Antivirals are most effective within the first 48 hours of symptoms, but doctors may still prescribe them later if the child is very sick or at high risk of complications. - Supportive treatment
If your child is dehydrated, they may receive IV fluids. If they’re struggling to breathe, they’ll be given oxygen. Medication may also be given to lower fever and relieve discomfort. Most children can go home after treatment, but if your child needs close monitoring or ongoing care, they may be admitted to the hospital.
Knowing what to expect at the ER can help you feel more prepared. Prompt medical care — especially when serious symptoms are present — can reduce the risk of complications and support your child’s recovery.
Common complications of the flu for children
Most children will recover from the flu without issues or complications. However, some may develop serious complications requiring hospitalization and further treatment. According to the CDC, in the 2024-25 flu season, at least 216 children died from a flu-related illness. This is the highest toll in over a decade.
“Most kids bounce back from the flu, but children with asthma, diabetes, or weak immune systems can become seriously ill very quickly. For them, even mild flu deserves close monitoring.” – Brian Knox, MD
Children with health conditions such as asthma, diabetes, or cystic fibrosis are at greater risk for complications from the flu. Even a typical case of the flu can quickly worsen in children with underlying conditions, which increases the chances of hospitalization or secondary infections such as pneumonia. If your child has any of these conditions, contact your pediatrician at the first sign of symptoms.
Serious flu complications in children include:
- Pneumonia: Viral pneumonia can lead to severe breathing issues in children and may result in hospitalization or ICU admission.
- Dehydration: The flu can cause dehydration due to high fever, vomiting, and reduced fluid intake. In extreme cases, this may require IV treatment.
- Sinus infections: Bacterial sinus infections may require antibiotics or even hospitalization in extreme cases.
- Ear infections: Ear infections are common in children with the flu and, in some cases, can lead to hearing loss when left untreated.
- Encephalopathy: Encephalopathy can cause rare but severe brain inflammation, seizures, confusion, and long-term brain damage.
- Myocarditis: This is a rare but serious inflammation of the heart muscle, which in the long term can affect normal heart function.
- Sepsis: A potentially life-threatening response to infection, sepsis affects the whole body and requires emergency care.
- Death: Death from flu complications is very uncommon, but most often occurs in children with underlying conditions.
- Asthma attack: The flu can trigger asthma attacks in children with asthma and may worsen respiratory symptoms, sometimes leading to hospitalization.
How Doctor on Demand can assist your child with the flu
If your child has flu symptoms, you can have a virtual visit with a board-certified provider through Doctor On Demand. If your child has a sudden fever, cough, fatigue, or if you’re simply concerned about a combination of flu-like symptoms, a Doctor on Demand video call can help determine whether those symptoms are signs of the flu and what treatment might be appropriate.
During your visit, the provider will:
- Review your child’s symptoms: Be prepared to discuss when symptoms started and the severity, including fever, cough, chills, fatigue, and trouble eating, sleeping, or breathing.
- Evaluate the likelihood of the flu: The doctor will consider your child’s symptoms to determine whether further testing is needed to determine whether your child has the flu, COVID-19, RSV, or the common cold.
- Advise on home care and further monitoring: You’ll receive personalized guidance on home treatment, including fever reducers, fluids, rest, and watching for the development of more serious symptoms.
Doctor On Demand is a convenient and reliable option for diagnosing and managing your child’s flu symptoms, especially when those symptoms are mild to moderate and home care is appropriate. If your provider has further concerns, they’ll help you determine how and when to seek additional care.
Need expert help managing your child’s flu symptoms? Sign up today and connect with a Doctor On Demand provider in minutes.
How to prepare for your Doctor on Demand visit for the flu
Before your virtual visit, make sure your device is charged and you’re in a quiet, well-lit space with a reliable internet connection. Write down when your child’s symptoms started, how they’ve progressed, and any key concerns. This will help you make the most of your time with the provider.
Here’s how to get ready for your child’s Doctor On Demand visit:
- Charge your device and test your setup
Make sure your phone, tablet, or computer is charged or plugged in. You can test your microphone, camera, and speakers in advance through the Doctor On Demand platform to avoid technical issues during the appointment. - Choose a quiet, well-lit space
Pick a space with good lighting so the doctor can see your child clearly. A quiet environment will help you focus and communicate openly without distractions. - Take note of symptoms and history
Write down when your child’s symptoms began and how they’ve changed — for example, fever patterns, energy levels, cough severity, breathing issues, or trouble drinking fluids. Include any known exposure to flu, COVID-19, or RSV, and note any underlying health conditions like asthma or diabetes. - Have your questions ready
Think about what you’d like to ask the doctor, such as whether your child needs flu testing, if antiviral treatment is appropriate, or what to watch for in the coming days. This helps ensure your concerns are fully addressed during the visit. - Have your child’s ID or your own ready
If medication is prescribed, you may be asked to verify your identity using a government-issued photo ID.
Doctor-answered children’s flu FAQs
This FAQ answers some of the most common questions about children’s flu, including when to take an immunocompromised child to the ER, why quick action is important for treating the flu, and what to feed a child who is sick with the flu.
“Starting treatment early can make a big difference. Antiviral medications are most effective within the first 48 hours, so don’t wait if your child is showing concerning symptoms.” – Brian Knox, MD
When should I take my immunocompromised child to the ER for flu?
If your child is immunocompromised, you should take them to the ER as soon as possible after the first sign of serious flu symptoms, including high, persistent fever, trouble breathing, lethargy, or dehydration.
Children with weakened immune systems are at a higher risk of complications related to the flu, and even moderate symptoms may warrant a medical evaluation.
How long does the flu last in children?
Flu symptoms typically last for 5-7 days in children. Early symptoms, such as fever and body aches, can resolve within the first several days, but fatigue and cough can persist for 1-2 weeks after other symptoms have subsided. The contagious period can last up to a week after the onset of symptoms.
Why is quick action important when a child has the flu?
Early treatment of the flu can shorten the overall duration of the illness, reduce the severity of its symptoms, and lower the risk of serious complications such as pneumonia, dehydration, and infection.
Young children and those with underlying conditions who are at particular risk of serious illness or complications should be seen as soon as possible.
How many children get hospitalized for the flu?
According to the CDC, between 7,000 and 26,000 children are hospitalized with flu-related complications each year. In years with severe flu outbreaks, hospitalization rates can increase significantly. While these numbers may seem high, it is important to remember that most cases of the flu in children can be treated at home with rest and fluids.
What should I feed my child with the flu?
A child with the flu should eat easy-to-digest foods and foods that aid in hydration. Simple carbohydrates, such as toast, crackers, rice, applesauce, and bananas, are a good basic diet to start with. Warm soups can help hydrate and provide more complex nutrition. Clear fluids like water, soup broths, and electrolyte solutions are excellent choices for hydration.
Avoid fatty or spicy foods, but generally speaking, your child can eat and drink what they crave and what they can digest, especially as they begin to get well.
When do flu symptoms peak in kids?
Flu symptoms usually peak between days 2 and 4 of illness, when fever, body aches, fatigue, and respiratory symptoms are most intense. After this peak, symptoms typically start to improve. Cough and tiredness may persist for several days but are usually signs of recovery, not worsening illness.
When can my child return to daycare after having the flu?
Typically, your child will no longer be contagious and can return to daycare 24 hours after their fever has resolved without the aid of over-the-counter fever-reducing medications. For their comfort, you may want to keep them home longer if other symptoms persist. Most children are ready to return to daycare 5-7 days after symptoms first appear.
How do you know when a child’s flu turns serious?
There are several signs that your child’s flu is serious enough to warrant further evaluation. Symptoms such as difficulty breathing, bluish lips or skin, severe fatigue, unresponsiveness, a high or persistent fever, or seizures are all signs that your child’s flu is more serious than normal.
When can a child go back to school after Influenza A?
A child can usually return to school once their symptoms subside and they have been fever-free for 24 hours without the use of fever-reducing medicines. Most children can return to school 5-7 days after they first exhibit symptoms.
Can my child get the flu after getting the flu vaccine?
Yes. Your child can still get the flu after being vaccinated. However, the vaccine or “flu shot” reduces the overall risk of infection and usually reduces the intensity of the illness, making it milder and shorter. Flu vaccines are updated yearly in anticipation of the most dominant strain. Vaccination remains the most robust defense against serious illness from the flu.
About the authors

Dr. Yvette Young is board-certified in Pediatrics and Pediatric Emergency Medicine with over twenty years of experience. She holds her medical degree from the University of Maryland and completed her residency and fellowship at Johns Hopkins, working at Level I trauma centers, including Children’s National Medical Center in Washington DC. In addition to her clinical work managing complex pediatric emergencies, Dr. Young has an MBA from Rutgers University, providing her with expertise in healthcare management, operations and strategic planning. She is a dedicated advocate for health equity and access to high-quality care for all children. Dr. Young lives in the Washington DC metro area with her family.

Dr. Brian Knox is board-certified in Internal Medicine and Pediatrics, and has been overseeing clinical services at Included Health for the past 3 years. Prior to joining IH 6 years ago, Dr. Knox spent 9+ years providing primary care to adults and children. He has expertise in preventive care, primary care for the LGBTQ+ population, as well as the management of patients with difficult-to-control diabetes and hypertension.



