Table of contentIn this article
- When to go to urgent care for a sore throat
- When to go to the ER for a sore throat
- When to use telehealth for a sore throat
- When you can’t wait to see your primary care doctor for a sore throat
- When to call 911 for a sore throat
- Questions to ask yourself before you decide to visit urgent care for a sore throat
- What typically happens during an urgent care visit for a sore throat?
- What can cause a sore throat?
- What can you do for a sore throat?
- What at-home treatments for a sore throat may doctors recommend until you seek treatment?
- What medications might doctors usually prescribe for a sore throat?
- How Doctor On Demand can assist with your sore throat right now
- Doctor-answered sore throat FAQs
Most sore throats heal on their own, but severe cases may require urgent care. Learn more about which symptoms mean you should go to urgent care or the ER, as well as when to use telehealth or see a primary care doctor. Plus, check out some home remedies that could help you feel better quicker.
When to go to urgent care for a sore throat
Go to urgent care if your sore throat is severe, lasts more than five days or comes with other symptoms like a high fever, swollen lymph nodes, or you have difficulty swallowing. Urgent care clinics provide quick diagnoses and treatments, including antibiotics if needed.
Most sore throats are common cases, so it can be hard to know when to seek urgent care or when to just rest at home. In fact, most sore throat symptoms resolve in three days for 60-70% of patients, according to March 2025 UpToDate, an evidence-based clinical decision support system used by healthcare professionals.
However, there are “Red Flag” symptoms that require urgent evaluation and management. These symptoms include: muffled or “hot potato” voice, drooling, any respiratory distress or trouble breathing, severe unilateral sore throat, stiff neck, neck pain or swelling, fever over 102°F (39°C), or history of recent injury to the throat. In these cases, an urgent care clinic might be the best option since it offers same-day appointments, extended hours, and immediate treatment.
Here’s a closer look at the red-flag symptoms that signal it’s time to visit urgent care for a sore throat:
- Severe sore throat or trouble swallowing
A severe sore throat or trouble swallowing suggests you might have a more complex underlying cause needing urgent medical attention. If symptoms of a sore throat don’t improve after five days, you should be evaluated in person.
- High and persistent fever (102°F/39°C or higher)
A high fever and a sore throat can indicate a more serious infection, such as strep throat.
- Swollen neck
Neck swelling may suggest an infection spreading into deeper tissues. If swelling appears on one side, it could be an abscess that needs urgent evaluation.
- Drooling or excessive saliva (difficulty swallowing)
Trouble swallowing, excessive drooling, or pooling saliva could mean a blocked airway or a severe infection. These symptoms require immediate medical attention.
- Shaking chills or night sweats
These symptoms indicate a systemic (body-wide) infection that might require urgent attention. Fatigue, joint pain, and an earache are other signs to watch out for.
- Severe pain below the jaw
Severe pain below the jaw might indicate swollen lymph nodes from a viral or bacterial infection. You might also feel a lump in your neck.
- Signs of dehydration
If swallowing hurts so badly that you’re not drinking fluids, you might start feeling the side effects of dehydration, which are dizziness, a very dry mouth, or dark urine. Dehydration can escalate quickly and needs prompt care.
- Changes in voice (“hot potato” voice)
Speaking in a muffled, strained voice, which some doctors call a “hot potato” voice, indicates severe swelling in the throat that needs medical attention.
- Difficulty breathing
If throat swelling narrows your airway, you may hear a harsh, grating noise when breathing (stridor). This is a serious sign of airway obstruction and requires immediate care.
When to go to the ER for a sore throat
Go to the emergency room (ER) if your sore throat causes any difficulty swallowing or breathing. This situation can be life-threatening and may suggest you have a serious infection, major swelling, or an allergic reaction that needs immediate care.
The ER is open 24/7 and has the equipment and staff to handle life-threatening conditions at any time. Unlike urgent care, which is suited for non-life-threatening conditions, the ER is designed to provide immediate, high-level care for severe complications from a sore throat, such as difficulty breathing, inability to swallow, or signs of a serious infection. If your symptoms are severe or rapidly worsening, the ER is the safest place for treatment, especially if it’s during a time of day when urgent care is closed.
Here are situations where the emergency room (ER) is the better choice over urgent care for a sore throat:
- Severe difficulty swallowing that makes it hard to drink water
If your throat pain is so intense that you cannot swallow even small sips of water, you may be at risk of severe dehydration. This symptom might indicate a serious infection, such as an abscess in your tonsils or swelling in your throat that could restrict your airflow. Severe dehydration often requires IV fluids, which ER staff can administer quickly.
- Trouble breathing or feeling like your throat is closing
If you are struggling to breathe, gasping for air, or feeling like your throat is tightening, it could be a sign of a severe allergic reaction (anaphylaxis), advanced infection, or airway obstruction. This is a medical emergency where you should call 911.
- Swelling in the throat or face that is worsening
Rapidly increasing swelling in the throat, tongue, or face can indicate a serious allergic reaction or a deep neck infection. This swelling can quickly block your airway, making it difficult to breathe. This is a medical emergency where you should call 911.
- High fever with extreme fatigue
A high fever above 103°F (39.4°C) may signal a serious systemic infection like mononucleosis, sepsis, or meningitis, especially if you’re also very confused or feel very weak and fatigued.
- Drooling due to inability to swallow
If you cannot swallow saliva and are drooling as a result, this could be a sign of epiglottitis, an inflammation of the tissue at the back of the throat that can rapidly close off the airway. This requires emergency treatment.
When to use telehealth for a sore throat
Telehealth offers a convenient way to treat a sore throat and also provides guidance when you’re unsure if you need in-person care. Through a video call, a doctor can assess symptoms, prescribe medication if needed, and suggest home treatments.
Here are some situations where telehealth is a good option for your sore throat:
- Your sore throat is mild, but you want professional advice
If your sore throat is bothersome but not severe, a telehealth visit can provide reassurance and guidance on whether you need further care.
- You need guidance on over-the-counter medications or at-home remedies
A doctor can recommend the most effective treatments, such as pain relievers, throat sprays, or natural remedies, and help you avoid unnecessary medications.
- You suspect strep throat
If you’ve had strep throat before and recognize the symptoms, if you’ve been exposed to someone with strep, or if you have a positive home strep test, a telehealth provider can discuss your history, assess your risk, and may prescribe antibiotics if appropriate.
- You have a sore throat linked to acid reflux
If your sore throat gets worse after eating, it might be related to acid reflux. A doctor can help identify triggers, suggest lifestyle changes, and recommend medications to manage symptoms.
- You want to avoid an in-person visit
If you want to reduce exposure to germs or simply avoid a trip to urgent care, telehealth is a convenient first step to evaluate your symptoms.
When you can’t wait to see your primary care doctor for a sore throat
It’s usually safe to schedule a routine visit with your primary care doctor for a mild sore throat if you don’t have serious symptoms like a high fever or trouble breathing. If your symptoms get worse before your appointment, you may need to go to urgent care.
Since primary care offices often require scheduled appointments, your sore throat may resolve before your visit. However, if you develop red-flag symptoms like a high fever or chills, or your sore throat doesn’t get better after five days, urgent care may be a better option.
Here are situations where you can wait to see your primary care doctor for a sore throat.
- Mild sore throat that’s improving
If your sore throat is improving with at-home remedies, like rest and hydration, it’s a sign that your sore throat is resolving. You don’t need urgent attention.
- No fever or difficulty swallowing
Without these red flags, it’s typically safe to wait for an appointment.
- Likely allergies
If you have a history of allergy-related sore throats, you can usually manage symptoms with allergy treatments while waiting for an appointment.
- Chronic mild sore throats
Many people are prone to frequent sore throats that go away on their own. If this description fits your situation, an appointment with your primary doctor might be enough to discuss remedies.
If your symptoms get worse before your scheduled appointment — especially if you develop a high fever, worsening pain, or difficulty swallowing — seek urgent care instead.
When to call 911 for a sore throat
Call 911 if your sore throat causes severe trouble breathing or swallowing, especially if you feel that you can’t get to the ER or other medical help safely. Infections or allergic reactions can block your airway and lead to life-threatening complications. Paramedics can provide life-saving treatment on the way to the hospital.
Paramedics can provide immediate emergency interventions on the way to the hospital, including oxygen support and life-saving medications. If you are experiencing any of the following and feel too sick to travel, calling 911 is the safest option:
- Respiratory distress
If someone is struggling to breathe or swallow, call 911 immediately. Extreme signs include gasping for air, visibly straining the neck forward to breathe, or significant drooling due to an inability to swallow. A muffled or weak voice may indicate a dangerously obstructed airway. In severe cases, lack of oxygen can cause loss of consciousness, which can lead to life-threatening complications if not treated right away.
- Severe sore throat with a fever of 102°F / 39°C or higher
A high fever with intense throat pain could indicate infections that can rapidly obstruct breathing. If swallowing is extremely painful and the fever is high, you may not have enough time to get to the ER safely without emergency transport.
- Significant swelling on one side of the throat
Swelling on just one side of the throat may be a sign of a peritonsillar abscess, a serious bacterial infection that can rapidly block the airway. Other symptoms include severe pain, difficulty swallowing, an earache, and a hoarse voice.
- If you have a compromised immune system and worsening symptoms
Infections can become life-threatening much faster if you have a condition that weakens your immune system, such as HIV/AIDS, cancer, or diabetes, or if you are on immunosuppressive medications (e.g., chemotherapy or steroids). Even a sore throat or mild infection could escalate into a medical emergency. Seek medical care immediately if you develop worsening symptoms, difficulty breathing, or signs of sepsis, such as confusion, rapid heart rate, or extreme fatigue.
Questions to ask yourself before you decide to visit urgent care for a sore throat
Before going to urgent care, consider key questions. How long have you had a sore throat? Do you have a fever or trouble breathing? Could allergies, food, or another factor be the cause? These answers help determine if urgent care is the right choice.
Consider these key questions to determine if you need immediate medical attention or if your sore throat can wait for a primary doctor or telehealth visit.
| Question | If Yes – Go to Urgent Care | If No – Consider Other Options |
|---|---|---|
| Has your sore throat lasted more than three days? | Prolonged sore throats may indicate a bacterial infection or another medical issue. | A short-term sore throat may resolve on its own — monitor symptoms or consult a primary care doctor. |
| Is your sore throat severely painful and not responding to pain medication? | Persistent, severe pain could indicate an abscess or another serious condition. | Mild or improving pain may not require urgent care — rest, hydration, and pain relievers may help. |
| Do you see white patches, pus, or an unusual rash? | These could indicate strep throat, scarlet fever, or another infection needing treatment. | A sore throat without these signs is more likely viral and may improve with self-care. |
Do you have a high fever (above 102°F / 39°C)? | A high fever may signal a bacterial infection needing medical attention. | No fever or a low-grade fever suggests a viral infection or mild irritation. |
| Do you have a weak immune system (e.g., due to chemotherapy, diabetes, or autoimmune disease)? | Weakened immune systems increase the risk of complications — seek care sooner. | If your immune system is healthy, you may be able to wait and monitor symptoms. |
If you experience difficulty breathing or swallowing, or if you notice swelling in your neck or face, Dr. Melissa Eirich, MD, a board-certified emergency medicine provider at Doctor On Demand® by Included Health with over three decades of experience, recommends going directly to the Emergency Room instead of urgent care.
What typically happens during an urgent care visit for a sore throat?
During an urgent care visit for a sore throat, you’ll describe your symptoms and how long they’ve lasted. The provider examines your throat, may perform tests like a strep test, and diagnoses the cause. Then, they’ll prescribe treatments, such as antibiotics or other remedies.
Here’s what to expect during an urgent care visit for strep:
- Patient history and a physical examination
First, a nurse or doctor will ask you questions about your sore throat, like when it started, how much it hurts, and whether you have other symptoms. Then, they’ll perform a physical examination. Usually, a medical professional will use an instrument with a light to see clearly into the back of your throat. They’ll check for swelling, redness, pus, or signs of infection. They may also feel your neck and ears to check for swollen lymph nodes.
- Diagnostic tests
Doctors usually start with a rapid strep test to check for Streptococcus pyogenes, the bacteria that causes strep throat. This test detects bacterial antigens and provides results within a few days. However, because it sometimes gives false negatives, doctors may perform a throat culture if symptoms strongly suggest strep. They use a sterile swab to collect a sample from the back of the throat and send it to a lab, where technicians grow the bacteria to confirm the infection. This two-step approach helps doctors quickly diagnose strep throat while ensuring they don’t miss cases that the rapid test fails to detect.
If your symptoms don’t indicate strep throat, doctors may run additional tests to identify other possible causes like viral infections from mono, the flu, or COVID-19.
- Treatment
After diagnosing the cause of your sore throat, the doctor will prescribe treatment. If the infection is bacterial, they may prescribe antibiotics. However, antibiotics have side effects, and their overuse contributes to antibiotic resistance, a growing public health concern.
Because of this, some doctors are moving toward a more structured approach to deciding when antibiotics are necessary. Here are two examples:
- Researchers demonstrate this shift in thinking in a 2023 study in the journal Infectious Diseases, titled “Best Management of Patients with an Acute Sore Throat – A Critical Analysis of Current Evidence and a Consensus of Experts from Different Countries and Traditions.” The authors describe a triage system that helps doctors balance the immediate need for antibiotics in high-risk cases — such as those at risk for rheumatic fever from strep throat — against the broader goal of reducing unnecessary prescriptions. Their framework categorizes patients based on clinical indicators such as symptom severity, the likelihood of bacterial infection, and individual risk factors for complications.
- In the 2014 paper from the journal Infectious Diseases, “Antibiotic prescription strategies for acute sore throat: a prospective observational cohort study,“ the researchers also suggest that many patients don’t need antibiotics. They also advocate for a “delayed prescription strategy,” where a doctor provides a prescription for antibiotics but advises the patient to wait before filling it and to only use the antibiotics if symptoms worsen or do not improve within a few days. This approach helps reduce unnecessary antibiotic use while still allowing treatment if the infection is bacterial and not improving on its own.
- Researchers demonstrate this shift in thinking in a 2023 study in the journal Infectious Diseases, titled “Best Management of Patients with an Acute Sore Throat – A Critical Analysis of Current Evidence and a Consensus of Experts from Different Countries and Traditions.” The authors describe a triage system that helps doctors balance the immediate need for antibiotics in high-risk cases — such as those at risk for rheumatic fever from strep throat — against the broader goal of reducing unnecessary prescriptions. Their framework categorizes patients based on clinical indicators such as symptom severity, the likelihood of bacterial infection, and individual risk factors for complications.
If your sore throat stems from another condition, such as tonsillitis, acid reflux, or a viral infection, doctors will take the appropriate next steps. Treatment might include pain relievers, antiviral medications, or lifestyle changes to address the underlying issue. Regardless of the cause, they will provide the best course of action to help you recover.
What can cause a sore throat?
Bacterial and viral infections, such as strep throat, mononucleosis, and COVID-19, cause many sore throats. Acid reflux, allergies, dry air, and irritants like smoke or pollution can also trigger throat pain. Less common causes include autoimmune disorders, vocal strain, and tumors in the throat or vocal cords.
Here’s a detailed list of conditions and factors that can cause a sore throat:
- Viral infections
Viruses, like the common cold and the flu, are a very common cause of sore throat. Usually, viral infections resolve on their own without treatment. At-home remedies can help soothe symptoms. However, if your symptoms are severe or don’t go away, visit a medical professional.
- Common cold: The common cold can cause a mild sore throat along with post-nasal drip, a headache, and a cough. There’s no cure for the common cold, but it usually goes away on its own.
- Flu: Influenza can lead to a more severe sore throat. Other flu symptoms include fever, joint pain, and fatigue.
- Bronchitis: Bronchitis is an inflammation of the bronchial tubes. It causes coughing, which can lead to a strained throat. Sometimes, you’ll see blood in your saliva or blood in your sputum (phlegm) after prolonged bouts of coughing. (See “When to see a doctor for chest congestion.”)
- COVID-19: Many COVID-19 cases start with a sore throat. You might also experience cough, fever, and loss of taste or smell. You can confirm with a COVID-19 test at home. Mild to moderate COVID-19 symptoms often resolve on their own in otherwise healthy people. However, people experiencing severe COVID symptoms or anyone who’s immune-compromised, should seek medical help. COVID-19 testing can help determine if it’s the cause of your sore throat.
- Mononucleosis (Epstein-Barr) Mono causes persistent sore throat, extreme fatigue, swollen glands, and sometimes an enlarged spleen.
- Common cold: The common cold can cause a mild sore throat along with post-nasal drip, a headache, and a cough. There’s no cure for the common cold, but it usually goes away on its own.
Bacterial Infection vs. Viral Infection
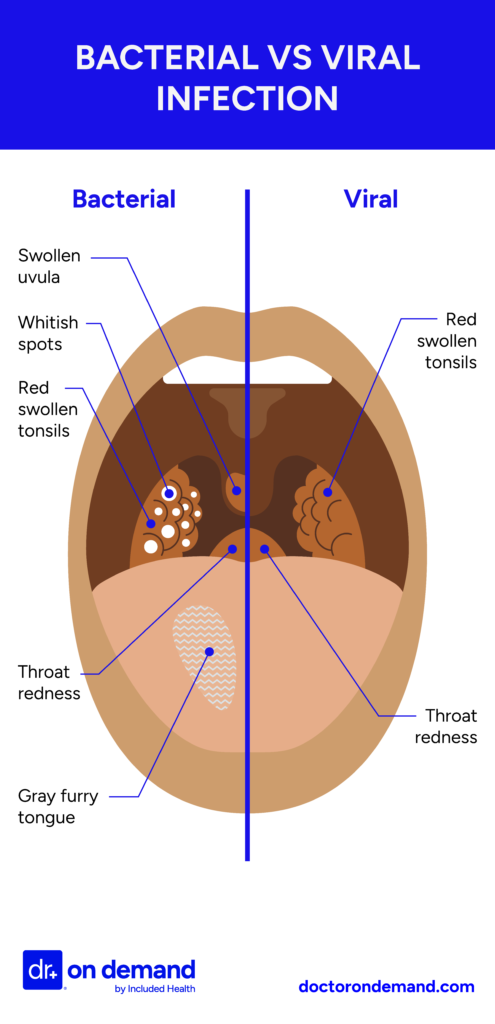
- Bacterial Infections
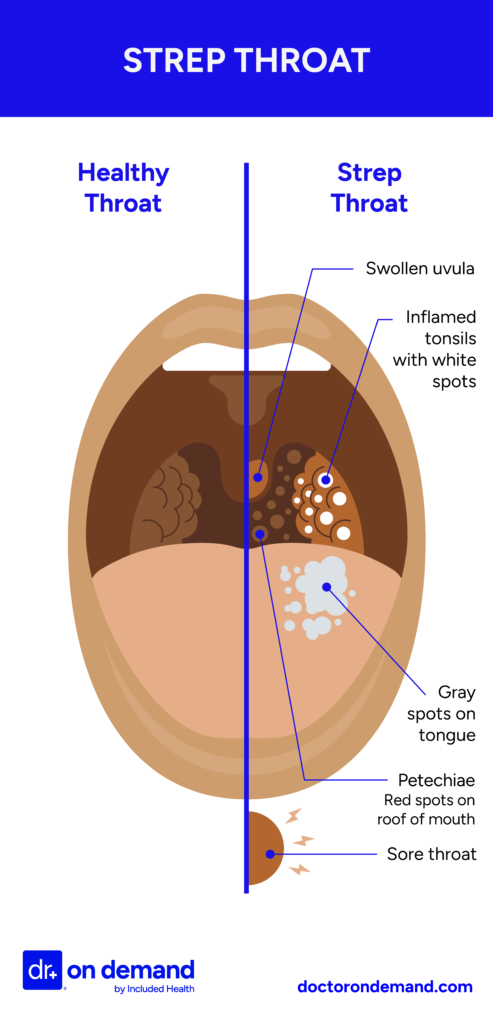
Bacterial infections occur when harmful bacteria enter the body and multiply, triggering an immune response, like a fever or even a sore throat. While some bacterial infections resolve on their own, many require medical treatment, such as antibiotics, to prevent complications and stop the infection from spreading.- Strep throat: Strep throat is a common bacterial infection that occurs when the bacteria Streptococcus pyogenes infects the throat and tonsils. It can lead to intense pain, fever, and white spots in the throat. There might also be tiny red spots on the roof of the mouth. Most people will need antibiotics to resolve strep throat.
- Epiglottitis: This serious infection causes the epiglottis, a flap of cartilage above your windpipe, to swell. The epiglottis is to prevent food and liquid from entering the lungs. This condition is a medical emergency that can cause extreme swelling that might potentially block an airway.
- Respiratory infection: Mycoplasma pneumoniae can cause a lung infection that can include persistent sore throat along with a dry cough and fatigue. This infection is most common in children between 5 to 15 years old. Only severe cases require antibiotics.
- Peritonsillar abscess: This complication of untreated tonsillitis creates a pus-filled swelling near the tonsils. It causes severe pain and difficulty swallowing.
- Strep throat: Strep throat is a common bacterial infection that occurs when the bacteria Streptococcus pyogenes infects the throat and tonsils. It can lead to intense pain, fever, and white spots in the throat. There might also be tiny red spots on the roof of the mouth. Most people will need antibiotics to resolve strep throat.
- Sexually transmitted infections (STDs/STIs)
Certain STDs can cause a sore throat. Seek STD testing immediately if you think you were exposed to one of these infections:
- Gonorrhea and Chlamydia: These bacterial infections can infect the throat, leading to soreness, redness, and pus-filled lesions. They are both treatable with antibiotics.
- Syphilis: Syphilis is a bacterial infection that can sometimes cause a sore throat. It is curable with antibiotics.
- Gonorrhea and Chlamydia: These bacterial infections can infect the throat, leading to soreness, redness, and pus-filled lesions. They are both treatable with antibiotics.
- Acid Reflux (GERD)
Gastroesophageal reflux disease (GERD) causes stomach acid to flow back into the throat and causes irritation. Usually, GERD requires changes in diet to avoid foods that trigger the symptoms, like spicy and fatty foods.
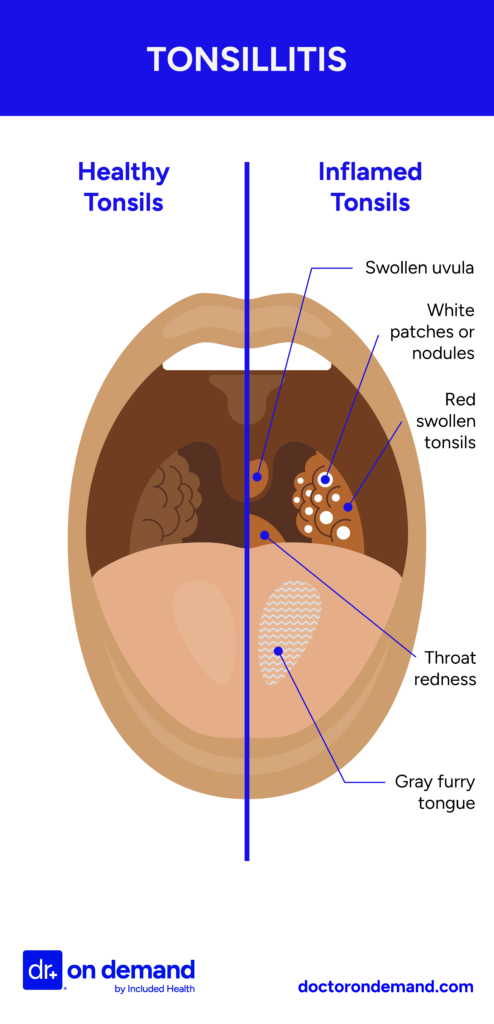
- Tonsillitis
Tonsillitis, or swollen tonsils, is inflammation related to bacterial or viral infections. Symptoms include throat pain, pus on the tonsils, swelling, and difficulty swallowing.
- Strep throat: Strep throat is a common bacterial infection that occurs when the bacteria Streptococcus pyogenes infects the throat and tonsils. It can lead to intense pain, fever, and white spots in the throat. There might also be tiny red spots on the roof of the mouth. Most people will need antibiotics to resolve strep throat.
- Epiglottitis: This serious infection causes the epiglottis, a flap of cartilage above your windpipe, to swell. The epiglottis is to prevent food and liquid from entering the lungs. This condition is a medical emergency that can cause extreme swelling that might potentially block an airway.
- Respiratory infection: Mycoplasma pneumoniae can cause a lung infection that can include persistent sore throat along with a dry cough and fatigue. This infection is most common in children between 5 to 15 years old. Only severe cases require antibiotics.
- Peritonsillar abscess: This complication of untreated tonsillitis creates a pus-filled swelling near the tonsils. It causes severe pain and difficulty swallowing.
- Overuse of straining your voice
Yelling, talking loudly for extended periods, or excessive singing can strain the vocal cords and lead to throat pain and hoarseness. Except for very severe cases, your throat and vocal cords just need rest to recover.
- Irritants
Exposure to certain substances like smoke, air pollution, or chemical agents like cleaning agents, can all inflame the throat. For example, swimming in a chlorinated pool can irritate your throat.
- Less common causes
Certain chronic conditions can cause a persistent sore throat, though they usually come with other distinct symptoms. Some autoimmune disorders can lead to throat irritation due to chronic inflammation or dryness. In rare cases, tumors of the throat, larynx, or esophagus can cause a severe, persistent sore throat. If a sore throat lasts for weeks without an obvious cause, seek medical attention.
Healthy Tonsils vs. Tonsillitis
What can you do for a sore throat?
You can ease a sore throat with home remedies and over-the-counter treatments while the underlying cause resolves. Drinking warm water, sipping tea with honey, or using a humidifier can help soothe the pain. Gargling salt water can help reduce swelling. Pain relievers like ibuprofen can also help.
What at-home treatments for a sore throat may doctors recommend until you seek treatment?
Doctors recommend drinking plenty of fluids, gargling warm salt water, using lozenges, taking pain relievers, resting your voice, and using a humidifier to ease throat pain. These treatments won’t cure the cause but can help with discomfort until you get treatment.
According to Dr. Melissa Eirich, MD, “It’s important to understand that sore throats can be caused by different things. While infections are a common cause, the treatment will depend on the specific cause. For many cases, especially those caused by viruses, you can find relief with some simple at-home treatments.”
Dr. Eirich recommends these at-home treatments for a sore throat:
- Salt Water Gargles: This is a really effective and easy remedy. Just dissolve half a teaspoon of salt in 8 ounces of warm water. Take a sip, tilt your head back, and gargle for about 15-20 seconds before spitting it out. You can do this every few hours to help reduce inflammation and soothe the pain.
- Honey: Honey has been proven in multiple studies to ease sore throats and coughs. Just a spoonful can help, but remember, it’s not suitable for children under one year old due to the risk of botulism.
- Throat Lozenges and Sprays: Over-the-counter medicated lozenges and sprays can numb the throat, providing temporary relief. Zinc lozenges are particularly good as they can also help reduce inflammation and might even shorten the duration of a viral infection.
- Pain Relievers: Common pain relievers like acetaminophen or ibuprofen are effective for reducing pain and fever. Just make sure to follow the dosage instructions on the bottle and check for any potential interactions with other medications you might be taking.
What medications might doctors usually prescribe for a sore throat?
Doctors prescribe antibiotics for a sore throat if it’s caused by a bacterial infection. For example, they might give you penicillin or amoxicillin for strep throat. For pain relief, they often recommend ibuprofen (Advil), acetaminophen (Tylenol), or lozenges.
According to Dr. Eirich, strep throat is less common and only accounts for about 5-15% of sore throat cases. It’s a bacterial infection and needs to be treated with antibiotics such as penicillin or amoxicillin to avoid secondary complications. If you’re allergic to penicillin, alternatives like azithromycin or a cephalosporin might be used. It’s important to complete the entire course of antibiotics to prevent the infection from returning or bacteria from becoming resistant.
Dr. Eirch adds that because strep bacteria can live on your toothbrush, changing your toothbrush midway through your antibiotic course and again at the end can help prevent re-infection.
For both viral and bacterial sore throats, doctors might prescribe an anti-inflammatory medication like ibuprofen or naproxen to manage pain and fever. If you’re given a prescription pain reliever, make sure to check with your doctor or pharmacist before combining it with over-the-counter pain medications to avoid any unwanted interactions.
Managing a sore throat effectively often involves a combination of home remedies and possibly medications, depending on the cause. Always feel free to ask questions and discuss your symptoms with your provider so they can provide the best care tailored to your needs.
How Doctor On Demand can assist with your sore throat right now
A Doctor On Demand virtual visit connects you with a board-certified provider in minutes, anytime you need help for your sore throat. Get an expert diagnosis, advice, and prescriptions — all available 24/7 from your home.
During your Doctor on Demand urgent care visit, your provider will assess your physical state, ask key questions, and determine the cause of your sore throat. Whether it’s the flu, strep throat, acid reflux, or certain STDs, they’ll provide a diagnosis and recommend the best treatment, including prescriptions if necessary. If in-person care is necessary, they’ll guide you on your next steps.
Sign up in minutes, skip the waiting room, and join the millions who have received expert care — all without the hassle of an in-person visit.
Skip the waiting room
Sign up in minutes and join the millions who have received expert care — all without the hassle of an in-person visit.
See a doctor nowHow to prepare for your Doctor On Demand visit for a sore throat
To prepare for a Doctor on Demand visit, set up your computer, laptop, or phone in a well-lit, quiet space for a clear video call. Jot down key details, including when your sore throat started, any symptoms, and possible triggers. Ensure a strong internet connection for a smooth visit and quick expert guidance.
Here’s a closer look at how to prepare for your virtual Doctor on Demand visit:
- Choose a quiet, well-lit space: Find a private, quiet location with good lighting to ensure clear communication with your doctor. Make sure your doctor can clearly see you and, if possible, use a high-resolution device so your doctor can properly observe your general appearance and assess your condition.
- Test your technology: Ensure that your internet connection and device are working properly. Test your device’s camera and microphone on the Doctor on Demand platform beforehand, and make sure your device is fully charged or plugged in.
- Gather any relevant medical information: Jot down key details about your symptoms, such as your sore throat history, and have a list of any medications you’re currently taking, including dosages. If you’ve recently had tests or treatments, have that information ready to share.
- List your questions: Mark down any specific questions or concerns you want to discuss with your doctor so you don’t forget them during the appointment. Consider asking about potential causes, recommended treatments, and any necessary follow-ups.
- Have a notepad handy: Take notes during the appointment to remember key points, including treatment recommendations, follow-up steps, or any lifestyle changes your doctor suggests.
Doctor-answered sore throat FAQs
Doctors answer frequently asked questions about sore throats, covering everything from causes to treatment. Find out if your sore throat is contagious, learn about symptoms to watch out for, and get advice on whether you should visit urgent care.
- Can urgent care look down my throat?
Yes, urgent care doctors check your throat with a light and tongue depressor. They look for redness, swelling, and other key symptoms like white or red patches.
- When do you need antibiotics for a sore throat?
You may need antibiotics if a doctor confirms your sore throat is caused by strep or another bacterial infection. Viral sore throats, like those from the flu or COVID-19, don’t respond to antibiotics and usually improve with rest, fluids, and over-the-counter pain relief.
- How do I know if my sore throat is serious?
Watch for red-flag symptoms like severe pain lasting more than five days, a high fever, or trouble swallowing. Other concerning signs include night sweats and swelling. If you’re unsure, it’s best to seek medical attention.
- What STDs cause sore throats?
Gonorrhea, chlamydia, and syphilis can cause a sore throat, particularly if you contracted the STD through oral contact. Herpes can also cause sore throats. A doctor can perform tests to determine the cause and recommend treatment.
- Should I go to a walk-in clinic or urgent care for a sore throat?
If your sore throat is severe and needs immediate attention, go to an urgent care clinic. If your symptoms are mild and haven’t lasted more than three to five days, a walk-in clinic or primary care appointment may be sufficient.
- Is my sore throat contagious?
It depends on the cause. Sore throats from viruses like the flu, strep throat, COVID-19, or STDs are contagious. But if it’s due to allergies, acid reflux, or other environmental factors, it’s not. A doctor can help determine the cause.
- Should I worry if I keep getting sore throats?
Frequent sore throats aren’t always a sign of a serious condition, but it’s worth consulting a doctor to identify the cause. Recurring sore throats can result from infections, allergies, acid reflux, or other factors. A doctor can rule out serious issues and recommend treatment.
- How to tell if a sore throat is viral or bacterial?
Viral sore throats often come with a cough, runny nose, or congestion, while bacterial infections like strep throat usually cause severe pain, swollen tonsils, and fever without cold symptoms. A doctor can confirm with a throat swab and recommend the right treatment.
- What is a red flag for a sore throat?
Red flags for a sore throat include difficulty breathing, swelling in the neck or face, chills, a high fever, or pain that doesn’t improve with over-the-counter medication. If you experience these symptoms, go to urgent care to rule out serious conditions.
- How long does a sore throat last with tonsillitis?
An acute sore throat from tonsillitis usually lasts one to two weeks. If symptoms persist beyond two weeks or don’t improve, consult a doctor to rule out complications or other underlying conditions.
Get treated for your sore throat now
Sign up in minutes and join the millions who have received expert care — all without the hassle of an in-person visit.
Online doctors available 24/7About the authors

Board-certified in emergency medicine, Dr. Melissa Eirich brings over three decades of clinical experience to her practice. Prior to joining Doctor On Demand in 2019, Dr. Eirich dedicated over ten years as an associate professor of clinical emergency medicine at the University of Rochester in New York and also worked in urgent care settings. In addition to her clinical practice, Dr. Eirich maintains a significant focus on medical education at Included Health.

Adrian Black-Seitz has worked as a copywriter and blogger for over three years in the healthcare industry. He lives and works in Virginia and is passionate about the work Included Health is doing.

Dr. Heather Hockenberry is board certified in family medicine. She earned her doctor of medicine degree at the University of Nevada Reno School of Medicine where she also completed her internship and residency in family medicine, serving as chief resident during her time there. As an urgent care physician for a decade prior to coming to Included Health, she treated acute illnesses and injuries of a diverse nature in a clinic setting. She came to Included Health in 2015 as a staff physician, and currently serves as an associate medical director supporting our clients from a clinical perspective.



